Piriformis Syndrome FAQs
Piriformis Syndrome Causes, Diagnosis, and Treatment
Written By DR CHOW Hung-Tsan
(Last updated on: Novemebter 4th 2021)
What is Piriformis Syndrome?
The term Piriformis Syndrome can be used to describe both buttock pain arising from the Piriformis muscle and sciatica owing to compression of the Sciatic nerve by the Piriformis muscle [1].
It’s a poorly-understood condition in which the Piriformis muscle, located in the buttock, can ‘cramp up’ and causes buttock pain. The Piriformis muscle can also irritate the nearby Sciatic nerve and cause pain, numbness and tingling along the back of the leg and into the foot (the symptom of sciatica).
Recently, with improved understanding of the anatomy of the pelvis, especially from hip arthroscopy and magnetic resonance neurography, other causes of buttock pain with nerve symptoms have been identified, and the term Deep Gluteal Syndrome [2] has been proposed to replace the term Piriformis Syndrome– however the term ‘Piriformis Syndrome’ is well-established and probably best used for the time being.
Treatment for Piriformis Syndrome
Almost every treatment approach for Piriformis syndrome will include a focus on carefully and progressively stretching the Piriformis muscle.
Once a working diagnosis of Piriformis Syndrome is made, it’s appropriate to try a course of physical therapy, as physical therapy is often very effective, even in cases with long-standing symptoms.
If a patient fails to improve significantly with physical therapy, it’s appropriate to investigate further, to try to make sure nothing has been missed.
If the diagnosis remains ‘primary’ Piriformis Syndrome, it’s appropriate to consider second and third line treatments, such as injection.
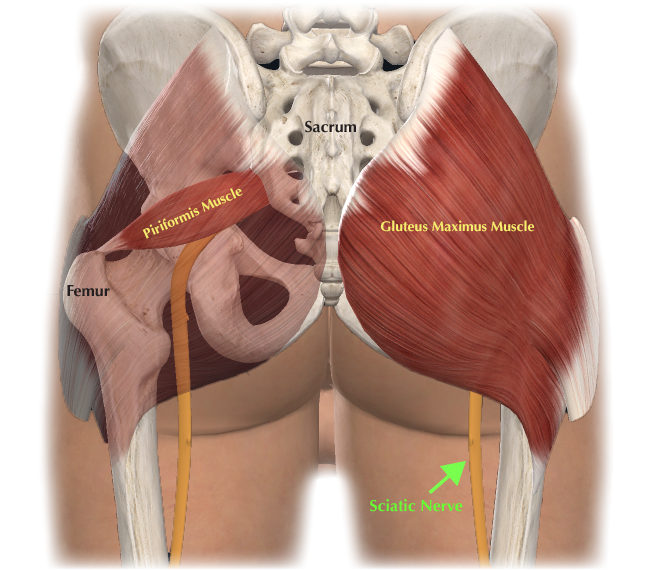
Fig. 1 Piriformis Muscle and Sciatic Nerve (Green Arrow) |
Where is the Piriformis Muscle? What does it do?
There are two Piriformis muscles, one in each buttock.
They are roughly triangular – similar to pyramids - in shape – hence the name.
They are medium-sized muscles, located deep in the buttock, beneath the Gluteus maximus muscle.(fig.1)
They start mostly at the sacrum (lower spine) and connect to tip of each femur (thigh bone), running approximately horizontally.
The Sciatic Nerve(fig.1), the major nerve supplying most of the lower limb muscles, usually runs just deep to Piriformis, which is why Piriformis problems can cause Sciatic symptoms.
Sometimes the Sciatic nerve can run through, or above, the Piriformis muscle, or the sciatic nerve may be split into two bundles with various unusual relations to the Piriformis[3, 4].
The ‘primary’ function of Piriformis is external rotation of the hip - assisting in turning the leg and foot outward – but Piriformis has secondary functions depending on the position of the leg – with the leg flexed it functions as an abductor of the hip – helping to stabilise the pelvis at heel strike – and would work hard climbing stairs. The secondary function is probably more important in everyday life than the primary function, but, however defined, the Piriformis muscle will be working whenever we walk, run, or climb stairs.
What are the causes of Piriformis Syndrome ?
The exact causes of Piriformis syndrome are unknown. Suspected causes include:
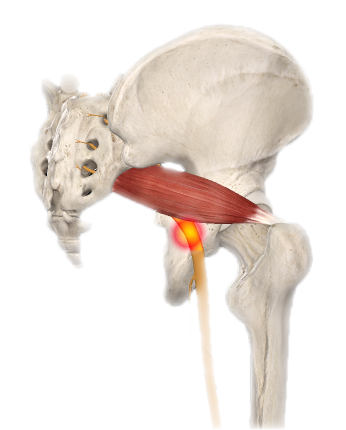
- Muscle spasm in the Piriformis muscle, either because of irritation in the Piriformis muscle itself, or irritation of a nearby structure such as the sacroiliac joint or hip.
- Tightening of the muscle, in response to injury or spasm.
- Swelling of the Piriformis muscle, due to injury or spasm.
- Bleeding in the area of the Piriformis muscle.
Any one or combination of the above problems can affect the Piriformis muscle (causing buttock pain) and may affect the adjacent Sciatic nerve (causing pain, tingling, or numbness in the back of the thigh, calf, or foot).
Fig 2. Piriformis muscle swellen that affect the Sciatic nerve |
How to make diagnosis of Piriformis Syndrome?
There is no simple diagnostic test for Piriformis syndrome. The condition is diagnosed on the basis of the patient’s symptoms and physical examination, and by excluding other causes of the symptoms, usually by investigations. Piriformis syndrome is often a diagnosis made through a process of ruling out other possible conditions that may be causing the patient’s symptoms.
Medical history
A medical history includes an in-depth review of the patient’s symptoms, such as what positions or activities make the symptoms better or worse, how long the symptoms have been present, if they started gradually or after an injury, and what treatments have been tried.
It will also include a review of conditions that may be in the patient’s family, such as arthritis.
Symptoms of Piriformis Syndrome
- A dull ache in the buttock
- Pain down the back of the thigh, possibly into the calf and foot (sciatica)
- Pain walking upstairs or inclines
- Increased pain after prolonged sitting
- Tightness of the hip joint
- May feel better lying down
- May have begun with an injury or unusual activity
Physical examination
The physical exam will include an examination of the spine, hips and legs to see what hurts, and what reproduces symptoms. Tenderness of the Piriformis muscle is usually a feature of the diagnosis.
A common way to examine the Piriformis muscle is for the patient to lie on their good side, and bend their sore leg about 90º, and the examiner presses along the course of the Piriformis muscle in the buttock. If this reproduces the patient’s pain, and pressing on the other buttock muscles does not, this confirms that the Piriformis muscle is painful. This may also cause symptoms along the Sciatic nerve, which lies beneath the Piriformis muscle, and will be compressed during the examination.
Investigations
X-rays and other spinal imaging studies cannot detect reliably detect Piriformis muscle spasm and if the Sciatic nerve is being irritated at the Piriformis muscle. However, diagnostic tests (including: blood tests for inflammation; X-rays of the pelvis; MRI of the hip and pelvis; and nerve conduction tests) may be conducted to exclude other conditions that can cause similar symptoms to Piriformis syndrome.
The most accurate method of looking at the Sciatic nerve in the region of the Piriformis is by the special MRI technique of Magnetic Resonance Neurography which attempts to produce high resolution images of the nerve.
An injection of local anaesthetic into the Piriformis muscle may help to confirm if the Piriformis muscle is the source of the symptoms.
Differential Diagnoses: What else could it be?
- Hamstring tendon problems – typically cause pain sitting and in the back of the thigh.
- Sacro-Iliac Joint problems – can cause a variety of symptoms, including buttock and thigh pain [5].
- Back problems – can cause a variety of symptoms, including buttock and thigh pain.
- Hip problems – can cause a variety of symptoms, including buttock and thigh pain.
- Tumour – either a benign swelling like a hernia [6] or a cancer - can cause almost any symptoms.
- Infection – can cause almost any symptoms. Usually blood tests will be abnormal.
- Inflammation – can cause almost any symptoms. Usually blood tests will be abnormal.
- Wallet neuritis [7] – compression of the Sciatic nerve from sitting on a bulky wallet.
Treatment options for Piriformis Syndrome:
Almost every treatment approach for Piriformis syndrome will include a focus on carefully and progressively stretching the Piriformis muscle.
- First Line: Once a working diagnosis of Piriformis Syndrome is made, it’s appropriate to try a course of physical therapy, as physical therapy is often very effective, even in cases with long-standing symptoms. If a patient fails to improve significantly with physical therapy, it’s appropriate to investigate further, to try to make sure nothing has been missed.
- Second and Third Line: If the diagnosis remains ‘primary’ Piriformis Syndrome, it’s appropriate to consider second (Oral medication)and third line treatments, such as injection.
- Fourth Line: Botox injection
- Fifth line: Surgical release or resection
First line:
Stretches for Piriformis Syndrome?
A number of stretching exercises for the Piriformis, hamstrings and hip extensors may help decrease the painful symptoms along the Sciatic nerve and return the patient’s range of motion.
Piriformis stretches There are a number of ways to stretch one’s Piriformis muscle. Two simple ways include:
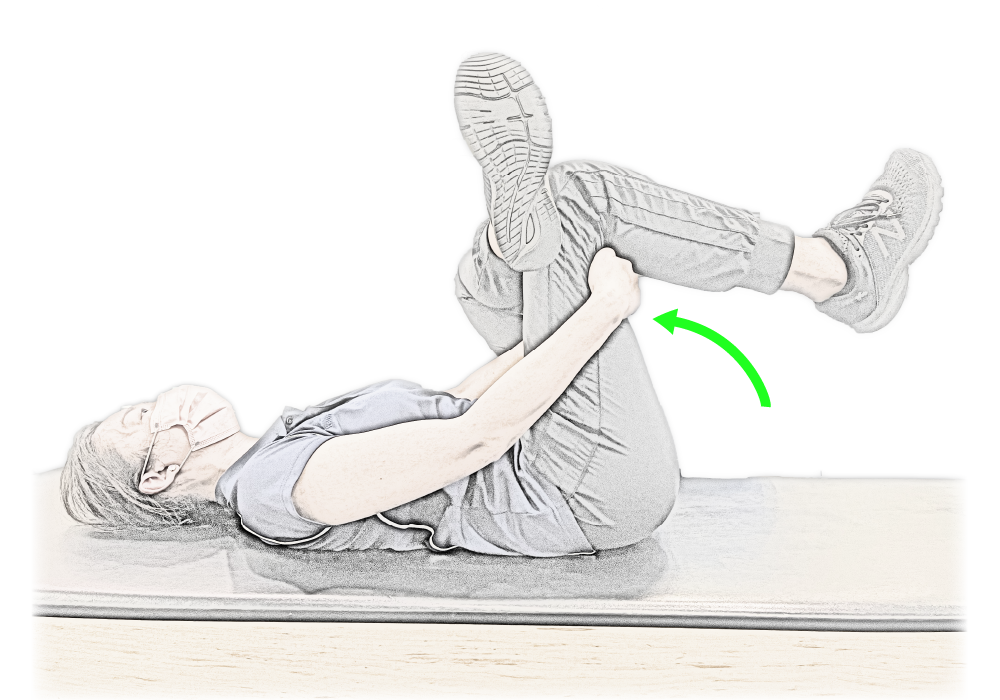
- Lie on the back with both feet flat on the floor and both knees bent. Rest one ankle on the opposite knee, place both hands just below the knee and pull the thigh towards the chest and hold the stretch. Repeat for the other side. (Fig 3a)
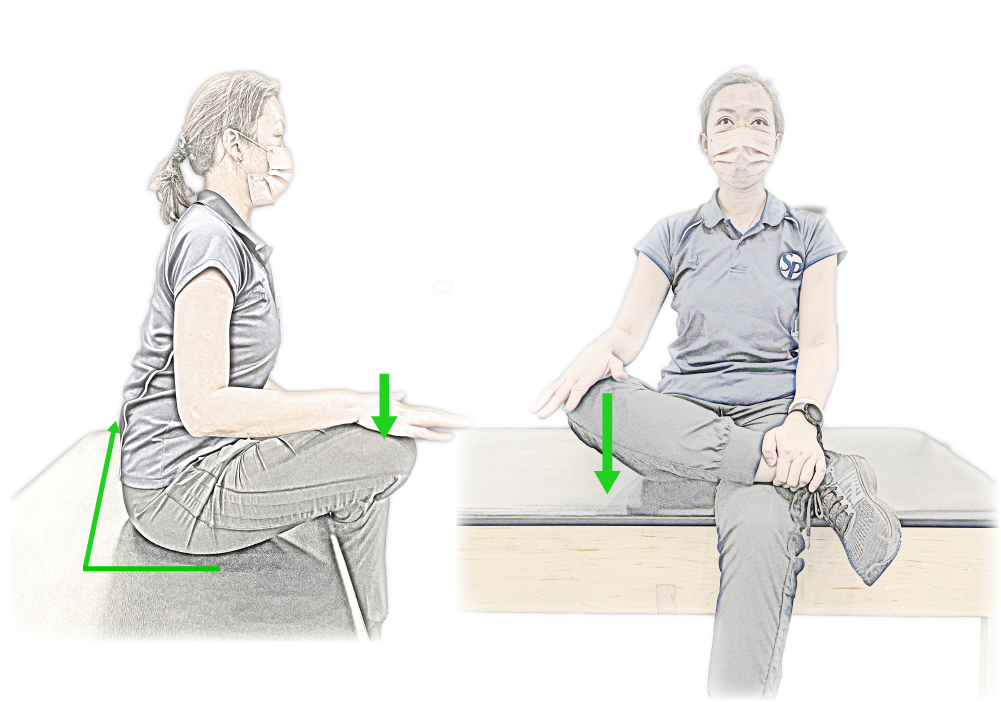
- Seat up straight, rest one ankle on the opposite knee (cross leg position), place one hand on the ankle to support the body and the other hand rest on the top of the knee and push it down, body lean forward till you feel the stretch on your hip and hold the position. Repeat for the other side. (Fig 3b)
Each Piriformis stretch should be held for 5 seconds to begin with, and gradually increased to hold for 30 seconds, and repeated three times each day.
Fig 3a. Pirformis Stretch |
Fig 3b. Pirformis Stretch (seating position) |
Hamstring stretches Stretching the hamstrings (the large muscles along the back of each thigh) is important for Sciatic pain. There are a number of ways to stretch the hamstrings:
- Place two chairs facing each other. Sit on one chair and place the heel of one leg on the other chair. Lean forward, bending at the hips until a gentle stretch along the back of the thigh is felt, and hold the stretch.
- Lie on the back with both legs straight. Loop a towel around one foot. Pull the leg up straight until a mild stretch along the back of the thigh is felt.
Again, try to work up to holding each stretch for 30 seconds and repeat three times each day.
Physical Therapy for Piriformis Syndrome
In addition to basic stretching, a comprehensive physical therapy and exercise program can be developed for each patient’s individual situation. A physical therapist, stretch therapist, osteopathy, chiropractor or other qualified health practitioner can develop a customised programme of stretching and range of motion exercises to help stretch the muscle and decrease spasm.
- Deep massage (manual release) by a physical therapist or other qualified specialist is thought to enhance healing by increasing blood flow to the area and decreasing muscle spasm. Depending on the severity of the patient’s sciatica-type pain and other symptoms, a number of treatment options may be recommended by a health care professional. A comprehensive approach to managing Piriformis syndrome may include a combination of the following nonsurgical treatments:
- Ice Packs and Ice Massage: At the onset of pain, lie in a comfortable position on the stomach and place an ice pack on the painful area for approximately 20 minutes. Repeat as needed every 2 to 4 hours. It may be more helpful to combine a gentle massage with the ice. Lie on the stomach and have someone gently massage the painful area with a large ice cube. If ice is applied directly to the skin (instead of a cold pack), limit it to 8 to 10 minutes to avoid an ice burn. If specific activities are usually followed by increased pain, it may be a good idea to apply ice immediately following the activity.
- Heat Therapy Some people find it helpful to alternate cold with heat. If using a heating pad, lie on the stomach and place the heating pad on the painful area for up to 20 minutes. Be sure to avoid falling asleep on a heating pad, as this may lead to skin burns.
Electrotherapy for Piriformis Syndrome
The application of electrical stimulation to the buttock with a transcutaneous electrical nerve stimulation (TENS) unit or interferential current stimulator (IFC) can help to block pain and reduce muscle spasm related to Piriformis syndrome.
Shock wave therapy
High energy shock waves affect the nucleus of cells, and can cause them to change their protein production, potentially aiding healing. They are widely used in physical therapy for treating superficial tendons – for example the patellar tendon, which is just below the skin, and is easily reached with a shock wave.
Shock waves have been tried for Piriformis Syndrome, but results have not been published in a peer-reviewed medical journal – there is a single report of reasonable success reported at a conference [8].
Investigators in Taiwan are recruiting subjects (probably through 2023) for a trial of shock waves vs steroid injection [9].
Because the Piriformis muscle is deep inside the buttock, a special transducer has to be used, and most physical therapists don’t have the special transducer. The same transducer cannot be used on a superficial and a deep structure.
Second line:
Oral Medications
Since most episodes of pain include some type of inflammation, non-steroidal anti-inflammatory medications (NSAIDs), such as ibuprofen or naproxen, may help decrease inflammation in the affected area.
Third line:
Piriformis Injections Therapy
For severe sciatica pain from Piriformis syndrome, an injection may be part of the treatment.
Local anaesthetic with steroid injection: A local anaesthetic and corticosteroid may be injected directly into the Piriformis muscle to help decrease the spasm and pain. The purpose of an injection is usually to decrease acute pain to enable progress in physical therapy.
Fig. 4 Botox Injection |
Fourth line:
Botox injection For persistent Piriformis spasm that is resistant to treatment with anaesthetic/corticosteroid injections, an injection of botulinum toxin (e.g. Botox®), a muscle weakening agent, may be useful(fig.4). The goal of the injection is to help the muscle relax and help reduce pressure on the Sciatic nerve.
The goal with both injections is to help the patient progress with stretching and physical therapy, so that when the effect of the injection is over the muscle will be remain stretched and relaxed.
Fifth line:
Surgical Release or Resection
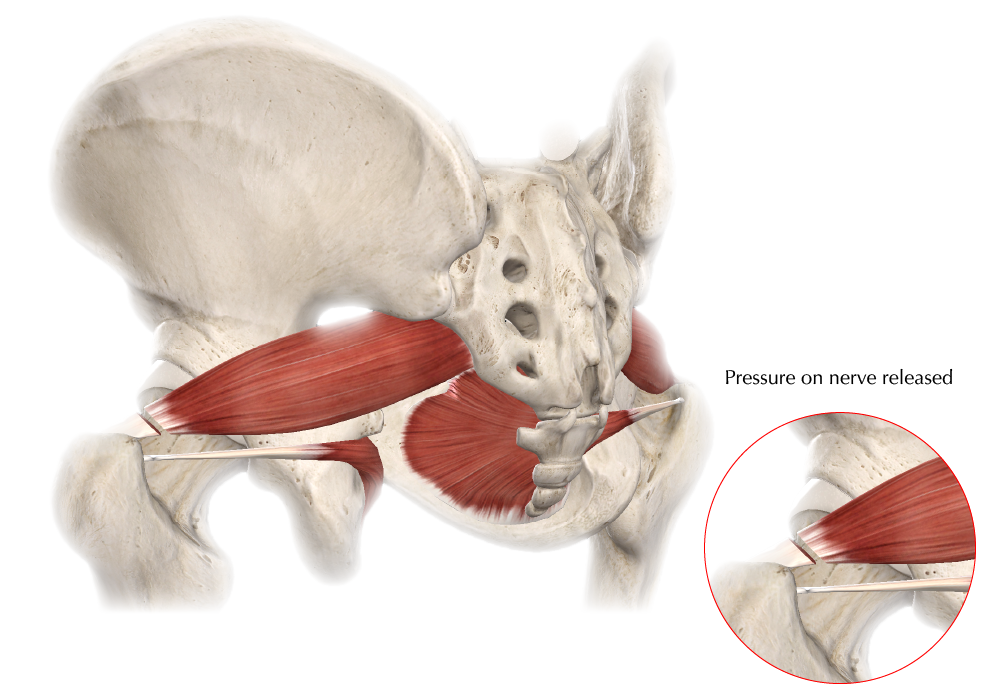
In persistent cases, the Piriformis muscle can be cut to relieve symptoms, and, though usually effective, this is rarely necessary. (fig.5)
Fig.5 an incision over the piriformis muscle to release the pressure on the sciatic nerve |
References:
- Hopayian, K., The clinical features of the piriformis syndrome. Surg Radiol Anat, 2012. 34(7): p. 671.
- Martin, H.D., M. Reddy, and J. Gomez-Hoyos, Deep gluteal syndrome. J Hip Preserv Surg, 2015. 2(2): p. 99-107.
- Beaton, L.E. and B.J. Anson, The relation of the sciatic nerve and of its subdivisions to the piriformis muscle. The Anatomical Record, 1937. 70(1): p. 1-5.
- Parsons, F.G. and A. Keith, Sixth Annual Report of the Committee of Collective Investigation of the Anatomical Society of Great Britain and Ireland. Journal of Anatomy and Physiology, 1896. 31: p. 31-44.
- Yoeman, W., The relation of arthritis of the sacroiliac joint to sciatica, with analysis of 100 cases. Lancet, 1928. 2: p. 1119-1122.
- Chitranjan, H. Kandpal, and K.S. Madhusudhan, Sciatic hernia causing sciatica: MRI and MR neurography showing entrapment of sciatic nerve. Br J Radiol, 2010. 83(987): p. e65-6.
- Siddiq, M.A.B., Piriformis Syndrome and Wallet Neuritis: Are They the Same? Cureus, 2018. 10(5): p. e2606.
- Huang, M.H., et al., Effects of Ultrasound-Guided Extracorporeal Shockwave Therapy on the Rehabilitation of Patients with Piriformis Syndrome. Ultrasound in Medicine & Biology, 2017. 43: p. S203-4.
- Effect of Ultrasound-guided Piriformis Muscle Corticosteroid Injection Versus Extracorporeal Shock Wave Therapy for Piriformis Syndrome: a Randomized Control Trial. Available from: https://clinicaltrials.gov/ct2/show/NCT04684537.
| Copyright @2021 Asia Medical Specialists Limited. All rights reserved. |