Acetabular Dysplasia FAQs
Acetabular Dysplasia FAQs
Written By Dr Jason BROCKWELL
(Last updated on: Oct 13th 2020)
What is Acetabular Dysplasia?
It is part of the condition known as 'Developmental Dysplasia of the Hip' (DDH), which was previously known as 'Congenital Dislocation of the Hip' (CDH).
The hip joint is a ball and socket joint. The ball is the head of the femur (thigh) bone, and the socket is formed in the pelvis, and is called the acetabulum (which means 'vinegar cup' in Latin, apparently from the shape of a Roman cruet set).
If the acetabulum (socket) is too shallow, the area transmitting one's bodyweight is too small, resulting in too much pressure on the articular cartilage, with subsequent failure, and arthritis of the hip joint.
Often both problems - acetabulum too shallow and facing the wrong way - occur together.
Two other commonly associated problems are to do with the shape of the femur:
1. it can have an incorrect amount of twist along its length ('version') and/or
2. the ball can be out-of-round, causing cam-type femoro-acetabular impingement.
Natural History
Diagnosis
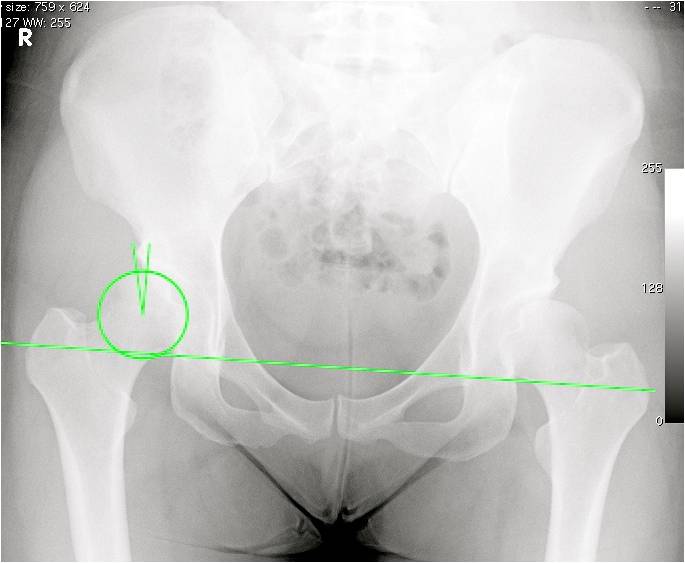 | |Fig. 1 AP X-ray of the pelvis and hips. Note the long green line representing 'horizon' is not level, and cannot be identified on an X-ray of only one hip. The circle outlines the femoral head, and the angle is the Centre-Edge angle of Wiberg (see text). In this case, both hips are dysplastic, with Centre-Edge angles below 15 degrees, and the right hip was painful. |
CT scan is very useful for defining acetabular version and femoral version, which requires cuts to be made through the knee as well. CT provides very high definition images of the bone.
MRI is also able to measure the important angles on the bones, though it does not produce quite as high definition of the bone, but it is also helpful for ruling out other causes of hip pain, such as avascular necrosis (AVN) of the femoral head, infection, tumours and some other problems.
Injection: Local anaesthetic +/- steroid +/- contrast into the hip joint may significantly reduce the pain, confirming the hip is the source of the pain (i.e. it is not coming from somewhere else, such as the back).
Classification
There are various methods, but the Centre-Edge angle of Wiberg [1] is probably most widely used as it is very easily measured from the AP pelvis X-ray. Normal >25 degrees; Borderline dysplasia: 20 – 25 degrees; Frank dysplasia <20 degrees.
Principal Differential Diagnoses (i.e. 'What else could it be?')
- Arthritis of the hip – this problem is more common in Caucasians
- Avascular necrosis (AVN) also known as 'osteonecrosis' of the femoral head (ONFH) – this problem is common in Asians
- Other causes of hip pain, such as Femoro-Acetabular Impingement
- Other causes of groin pain, such as a true hernia or 'sports hernia', pain from the back or SI joints, a 'groin strain' or adductor strain, osteitis pubis, a stress fracture, infection, tumour etc.
Treatment options
No treatment: Avoid impact, wear soft soled shoes, control body weight, take glucosamine 1.5 grams per day long term, take painkillers as needed, have steroid injections into the hips as needed, and accept the possibility or likelihood – depending on the severity of the dysplasia - of progression to arthritis.
Hip Arthroscopy ('keyhole surgery') to assess the joint prior to pelvic osteotomy and to provide temporary relief by cleaning the joint and possibly correcting some associated femoro-acetabular impingement. Arthroscopy cannot correct or cure acetabular dysplasia.
Pelvic osteotomy to correct the anatomy. This is the best treatment, but if the X-ray or arthroscopy shows the joint is already badly damaged it is probably too late, and one would probably be best to go for hip replacement. If the pelvic osteotomy eventually fails, it is easier to perform a hip replacement afterwards because the acetabulum is deeper, and more suitable for fixing the acetabular component of the replacement hip [2].
Hip replacement. New designs of hip replacement – especially hip resurfacings, such as the Birmingham Hip Resurfacing (BHR) – can offer a 'normal' hip, but we only have results for a little over 10 years – we do not know if they will last for life. Obviously it is better to save one's own hip than to replace it, if possible.
Pelvic Osteotomy
The term 'osteotomy' means 'cutting a bone'. This is an operation to correct the anatomy by cutting the pelvic bones so the acetabulum can be repositioned. If the thigh bone is incorrectly angled or twisted, this would be cut and corrected at the same time [3], which is called a 'femoral osteotomy'. If the ball was 'out-of-round' this would also be corrected at same time by a 'Heyman-type femoroplasty'.
Birmingham Pelvic Osteotomy
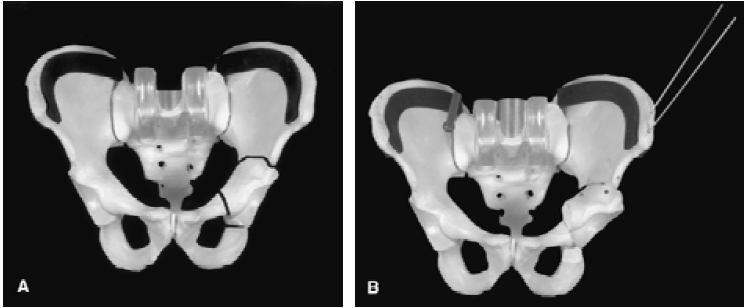
For most patients with acetabular dysplasia, Asia Medical Specialists recommend a 'Birmingham Pelvic Osteotomy'. This is also known as an 'Interlocking Triple Pelvic Osteotomy' because it involves cutting each of the three bones of the pelvis in such a manner that, when the acetabulum is repositioned, the cut bones 'lock' into a stable position [4]. This has the advantage that the operation is very reliable because the position of the acetabulum can be accurately controlled and will not change unexpectedly, and, because the bones are stable, the patient can bear weight on the operated leg (although one will need the help of crutches initially), and the cut bone heals quickly and reliably. This operation is similar to a 'Peri-Acetabular Osteotomy' (PAO) and has the same effect, though it differs slightly in the technical details. If a femoral osteotomy is performed at the same time, it is usually necessary to walk with the aid of crutches for at least 6 weeks, until the femur has healed.
|
X-ray technique for hip problems
Two specially positioned X-rays are required. In fact one is a 'standard' view, and the other is a slight modification of a standard view, so no special equipment or expertise is required.
X-ray number 1: AP pelvis & hips. This is a ‘standard’ X-ray of the whole pelvis and hips taken with the subject lying down. The legs are internally rotated 20 degrees to make the femoral necks parallel to the plane of the film. The beam is centred at the pubic symphysis at the level of the tips of the greater trochanters of the femora. The beam to film distance is 1 to 2 metres. On the film, one should check that the pelvis is not:
1. rotated - by seeing that the sacral spinous processes and the pubic symphysis, which are both in the midline, line up.
2. flexed or extended - by seeing that the tip of the sacrum is within 2 to 5 cm of the superior pubic rami.
X-ray number 2: Modified frog laterals both hips. This is a slight modification of the standard frog lateral in that the hips are not abducted (ie the legs spread apart) as much. The subject lies supine and the beam is centred in the same way as for the first X-ray, but the legs are bent up at the hips and the knees bent to 90 degrees. (Figs. 5A & B)
The feet are placed next to each other, with the soles flat on the table, and the legs are spread slightly (abducted 20 degrees from the vertical, for a total arc between the thighs of 40 degrees). (Fig. 5B)
On the film, one should check that the pelvis is not rotated by seeing that the sacral spinous processes and the pubic symphysis, which are both in the midline, line up, but the pelvis is expected to be flexed in this position.
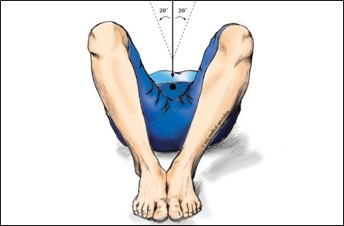 Fig. 5A Modified frog lateral X-ray: the beam is centred on the public symphysis.  Fig. 5B Modified frog lateral X-ray is taken with the legs only slightly apart and the soles of the feet flat on the X-ray table. |
References
1. Wiberg, G., The anatomy and roentgenographic appearance of a normal hip joint. Acta Chir Scand, 1939. 83(Suppl 58)(83(Suppl
58)): p. 7-38.
2. McBryde, C.W., et al., Metal-on-metal hip resurfacing in developmental dysplasia: a case-control study. J Bone Joint Surg Br, 2008.
90(6): p. 708-14.
3. Vallamshetla, V.R., E. Mughal, and J.N. O’Hara, Congenital dislocation of the hip. A re-appraisal of the upper age limit for treatment.
J Bone Joint Surg Br, 2006. 88(8): p. 1076-81.
4. Kumar, D., C.E. Bache, and J.N. O’Hara, Interlocking triple pelvic osteotomy in severe Legg-Calve-Perthes disease. J Pediatr Orthop,
2002. 22(4): p. 464-70.
| Copyright ©2017 Asia Medical Specialists Limited. All rights reserved. |