Shoulder Dislocation FAQs
Shoulder Dislocation FAQs
written by Dr Kelvin Tam
(Last updated on: April 22nd 2022)
.png?1715939527911)
What is Shoulder Dislocation?
The shoulder is a 'ball and socket' joint. The ball is the head of the humerus – and the humerus is the long bone in the upper arm. The socket is the glenoid fossa of the shoulder blade. The socket is shallow to allow a large range of motion. Hence, the shoulder is naturally unstable, and shoulder dislocations, when the ball comes out of the socket, are relatively common injuries.
These FAQs refer to the most common type of dislocation of the shoulder – where the ball comes out of the front of the socket, damaging the front of the socket. (This is called an 'anterior dislocation'.)
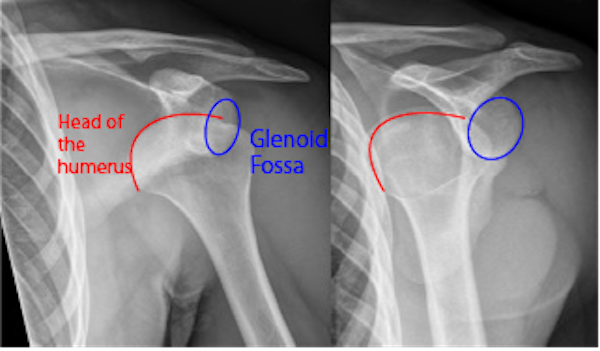 |
| Fig 1.X-ray of a dislocated shoulder. The ball and socket are outlined. |
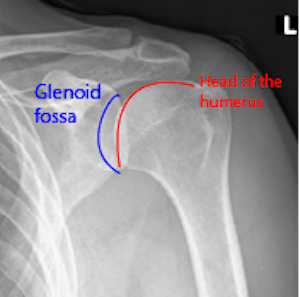 |
| Fig 2. X-ray of a normal shoulder. The ball and socket are outlined. |
Shoulder Dislocation Symptoms: will I know if I have dislocated my shoulder?
First-time shoulder dislocations are traumatic events. Typically, they occur with significant force, such as a sports injury or hard fall.
There will be much pain in the shoulder and arm, and the arm won't work because it is 'stuck' or 'locked'. The person with a dislocated shoulder will know something is badly wrong with their shoulder and they need help, but they typically won't know what the problem is.
Subsequent dislocations may occur with trivial injuries, and the pain will usually be less, though the arm still won't work while the shoulder remains dislocated. Patients having a second dislocation usually recognize the dislocation themselves.
How are shoulder dislocations diagnosed?
The majority of shoulder dislocations are easily diagnosed by a physiotherapist or doctor.
The story of injury and the characteristic deformity are diagnostic. However, an X-ray is essential to look for associated fractures. Sometimes, a CT scan is necessary to identify fractures not shown on ordinary X-rays. Magnetic resonance imaging is needed for those planning surgery as a 'road map'.
Treatments for dislocated shoulders
What is first aid?
Ideally, the patient will be taken swiftly to the hospital, an X-ray taken to check for fractures, and, if no major fracture, given enough pain relief to relax the muscles and allow the doctor to place the ball back in the socket gently. Putting the ball back in the socket by manipulating the arm is called 'closed reduction'.
In a wilderness environment, where hospital treatment is not rapidly available, or at a sports event where the on-field medical team arrives very quickly, it may be appropriate to perform a closed reduction in the field, and some individuals manage to reduce their dislocations
What happens next?
It depends on the exact injury.
Most 'fracture-dislocations' where the bone is broken and the joint dislocated need an operation. Fortunately, these are not the most common type of shoulder dislocation.
The most common injury in shoulder dislocation involves a 'soft tissue Bankart lesion', and these FAQs refer primarily to this.
Bankart lesions almost never heal properly on their own, and therefore the shoulder remains unstable.
Studies have shown that the redislocation rate is high and correlated with age and gender [1]:
- People 40 years and under are 13.5 times more likely to suffer recurrent instability following a first-time traumatic anterior shoulder dislocation than those over the age of 40 years.
- Men are 3.2 times more likely to suffer from recurrent instability following a first-time traumatic anterior shoulder dislocation than women (47.3% and 25.5%, respectively).
- Probably almost no shoulders spontaneously heal and self-stabilize, but older patients limit their activities to avoid redislocation.
What are the treatments for shoulder dislocation?
- Non-operative treatments -Non-operative treatment consists of wearing a sling for about six weeks in the hope of allowing the soft tissues to heal, followed by a rehabilitation programme to regain range of motion and strength, returning to normal activities after 3 - 6 months. In practice, most shoulders do not become stable.
- Surgery?: Almost everyone requires surgery:
- Patients whose dislocated shoulder cannot be put back in place by closed reduction – usually because some tissue is jammed in the joint - should have surgery performed as soon as possible.
- Dislocations with associated injuries, such as fractures or rotator cuff tears.
- For patients with repeated dislocations, their shoulders will definitely remain unstable.
- People with loose ligaments.
- People who are likely to suffer repeated dislocations – essentially anyone under 40 who is reasonably active.
What happens during a dislocation?
In the most common type of dislocation – anterior - where the ball dislocates out of the front of the socket, it usually knocks the cartilaginous labrum off the edge of the bony glenoid socket. The labrum acts to form a suction seal to stabilize the joint. If the seal is broken and the suction is lost, the shoulder becomes unstable. The labrum does not usually heal back to the glenoid, and the shoulder remains unstable. A London orthopaedic surgeon named Blundell Bankart realized the significance of this injury and did much to educate his colleagues [2]. Consequently, the detachment of the labrum from the glenoid is called a "Bankart lesion". When a bit of bone breaks off the glenoid with the labrum, we usually call it a "Bony Bankart".
Fig 3. The left MRI shows a normal right shoulder, which the red arrow shows the front part of the glenoid labrum – the small black triangle. It's firmly attached to the bony socket (called the 'glenoid').
The right image is an MRI of a recently dislocated (and reduced) right shoulder. The red arrow shows a 'Bankart lesion'– the labrum (the small black triangle) is surrounded by a white halo and is not connected to the bony glenoid. The white halo is a mixture of blood and joint lubricant fluid, which prevents the labrum from healing back to the glenoid – which is why dislocated shoulders usually remain unstable. The blue arrow shows a Hill-Sachs lesion – a divot in the back of the head of the humerus bone made by the front of the glenoid during the dislocation. Normally, in this particular MRI sequence, the bone should appear black, but the divot is surrounded by white, representing cracks and bleeding inside the bone.
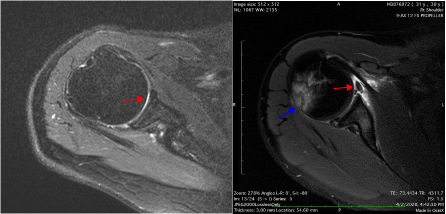 |
| Fig 3. Left shows a normal shoulder, Right: a dislocated right shoulder |
What does surgery involve?
Ideally, the patient should have a "Magnetic Resonance Arthrogram" for pre-operative planning. This is a normal MRI scan, with the addition of an injection of dye into the joint, to identify injuries which may not be shown on plain MRI but are important – especially 'HAGL lesions'
In most cases, surgery is performed arthroscopically ("keyhole surgery") using a video camera and tiny incisions, and the patient can go home from the hospital the next day.
It's usually possible to restore normal anatomy. The labrum is stitched back to the glenoid using 'bone anchors' and knots tied inside the joint using special instruments.
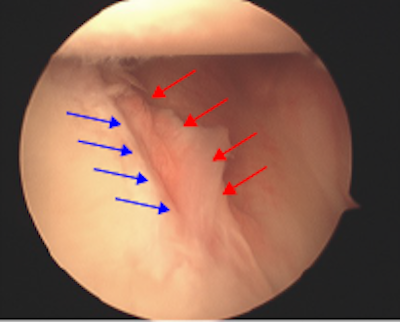 | 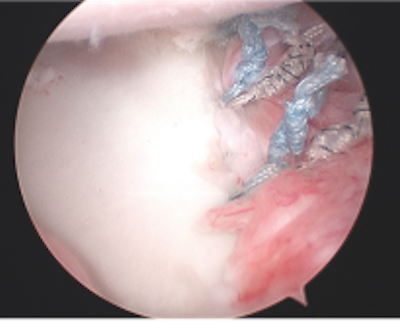 |
| Fig 4.Arthroscopic view of a Bankart lesion. There is a gap between the labrum (red arrows) and the edge of the glenoid bone (blue arrows). | Fig 5. Arthroscopic view of a Bankart repair. The labrum is stitched firmly to the glenoid bone. |
"Bony Bankart lesions" may require bone graft surgery, which is slightly more complex but can usually be performed arthroscopically [3] and gives good results. If an associated Hill-Sachs lesion is very large, then a "remplissage" procedure is performed at the same time to tighten up the back of the shoulder capsule, slightly reducing shoulder rotation and preventing the Hill-Sachs divot from catching and causing problems.
Post - Operation
How long does it take to recover?
There are three broad and slightly overlapping phases of recovery:
- Healing of the repair – it takes about 6 weeks for enough new collagen protein to strongly heal the soft tissues so that the labrum is attached to the glenoid by normal tissue instead of relying on the stitches.
- Regaining movement – the shoulder will become very stiff after the operation, and one cannot stretch too much as it is necessary to protect the repair until it is strong at 6 weeks, so initially, one does simple exercises, followed by more aggressive stretches from 6 weeks.
- Regaining strength and endurance – initially, one can only do simple exercises, but from 6 weeks, one can increase the challenge, hoping to recover about 90% strength and endurance by 3-6 months post-operation.
Full strength and endurance for demanding activities like serving in tennis, driving in golf etc., will take at least six months.
When can I return to work?
The recovery period for a patient depends on his job nature.
- Office workers: A few days.
- Drivers: At least 6 weeks.
- Pilots: Return to flying when the range of motion is sufficient to reach overhead controls and is strong enough to control the yoke – usually 3 months.
- Active-duty uniformed services officers (Police, Fire etc.): When able to reach the full range with good power – usually 4 – 6 months.
- Light manual workers, not requiring heavy or overhead lifting: about 3 months
- Heavy manual workers, requiring heavy or overhead lifting: about 6 months
When can I drive?
It is not safe for anyone to drive until at least 6 weeks after their operation – if one were to drive sooner and have an accident, one could be held criminally liable, and one's insurance company would not cover the costs.
What is rehabilitation?
One can go home the day after the operation; return to office work within a few days;
The patient needs to wear a shoulder immobilizer constantly for the initial two weeks for comfort and protection; then, it can be removed for dedicated exercises. However, the shoulder immobilizer should be used in the initial six weeks during outside home activities. One can type on a keyboard in the shoulder immobilizer. After the initial six weeks, the emphasis is on stretching until the shoulder regains full range of movement, and then muscle strengthening is encouraged. The overall process takes about 6 months.
Do I need physiotherapy?
Physiotherapy is very helpful and should be started 6 weeks after the operation and continued until the patient has achieved full recovery and returned to full sports or work demands—so up to 6 months [4].
Can I return to sports?
Yes. One can return to any sport. In order to return to any given sport, one needs to have a sufficient range of motions, strength, and endurance to perform the activity safely and reasonably well. Depending on the sport, full participation is usually 6 - 9 months after the procedure.
How successful is the operation?
Internationally, arthroscopic Bankart repair produces a 7-fold lower recurrence rate (about 10% vs 70%) and a higher rate of return to play (about 90% vs 80%) than non-operative treatment [5].
What are the disadvantages of operation?
The operation usually restores normal shoulder anatomy and function, so unless one has a complication (complications are unusual), there is no medium or long-term disadvantage.
Are there any foods or supplements that help or things to be avoided?
There are no foods or supplements that help shoulder instability. Take a normal healthy diet. There are no foods to avoid.
Smoking delays healing – it's not good to smoke when recovering from an injury or operation.
References:
- Olds, M., et al., Risk factors which predispose first-time traumatic anterior shoulder dislocations to recurrent instability in adults: a systematic review and meta-analysis. Br J Sports Med, 2015. 49(14): p. 913-22.
- Bankart, A.S.B., The pathology and treatment of recurrent dislocation of the shoulder joint. BJS (British Journal of Surgery), 1938. 26(101): p. 23-29.
- Campos-Mendez, A., J. Rayes, and I. Wong, Arthroscopic Anatomic Glenoid Reconstruction With Distal Tibial Allograft and Hybrid Fixation. Arthrosc Tech, 2022. 11(2): p. e163-e169.
- Gaunt, B.W., et al., The American Society of Shoulder and Elbow Therapists' consensus rehabilitation guideline for arthroscopic anterior capsulolabral repair of the shoulder. J Orthop Sports Phys Ther, 2010. 40(3): p. 155-68.
- Hurley, E.T., et al., Arthroscopic Bankart Repair Versus Conservative Management for First-Time Traumatic Anterior Shoulder Instability: A Systematic Review and Meta-analysis. Arthroscopy, 2020. 36(9): p. 2526-2532.
Articles written/edited/reviewed by Doctors of Asia Medical Specialists ©2022 Asia Medical Specialists Limited. All rights reserved. |
