Chronic Ankle Instability FAQs
Chronic Ankle Instability FAQs
written by Dr SW KONG
Last update: Aug 24th 2020
What is chronic ankle instability?
Chronic ankle instability is the feeling that the ankle is “weak” or “loose” or “gives out” or feels “unstable”. It is a common problem following an ankle sprain: up to 40% of people who badly sprain an ankle go on to have repeat sprains, and symptoms of instability.
Picture showing acute inversion injury of right ankle, red arrows indicate bruise and swelling.

How does the ankle joint work?
The ankle joint is a complex hinge joint between the leg and foot.
Ligaments: strong bands of fibrous connective tissue that connect the bones together. On the outer side of the ankle joint, there are three ligaments (see Figure 1). The one at the front called the ‘Anterior Talo-Fibular Ligament’ (ATFL) is the most commonly injured in ankle sprains.
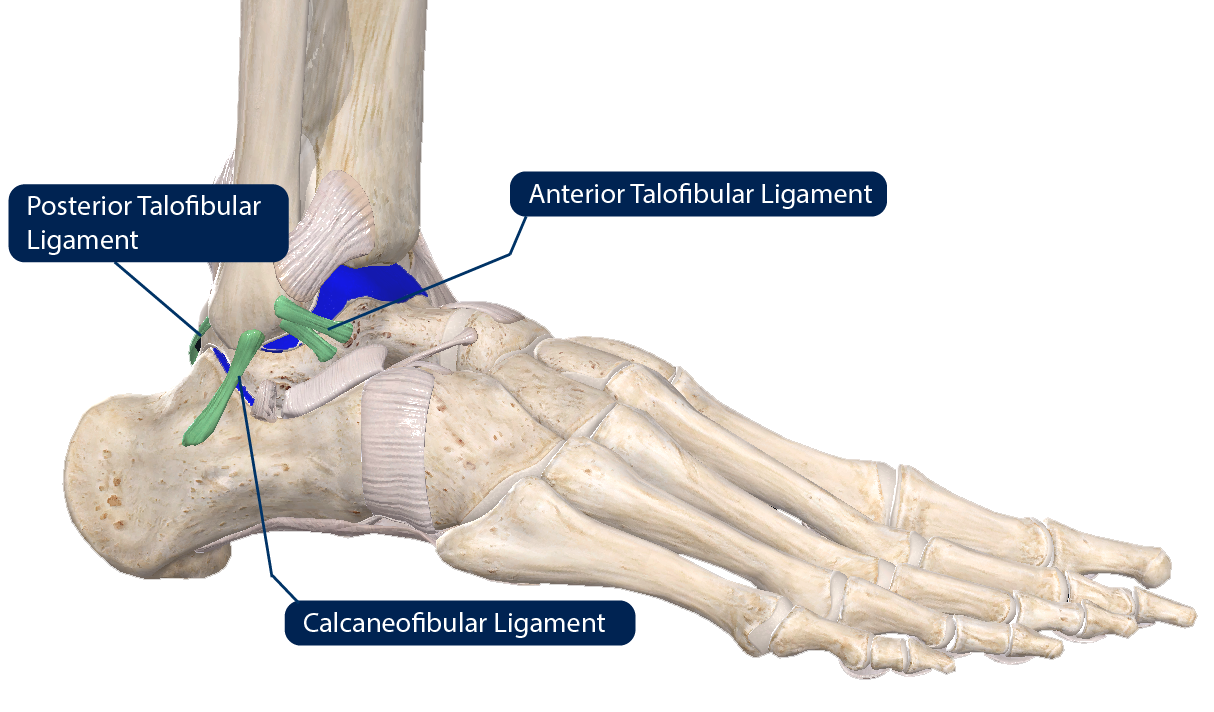 |
| Figure 1: Outside of the right ankle joint. The three ligaments are coloured green and cartilage blue. Anterior Talo-Fibular Ligament is most commonly injured in a sprain. At the same time, the cartilage can also be injured in certain situation. |
What are ankle sprains?
Injuries to ligaments are known as ‘sprains’. Sprains are classified into mild, moderate, and severe (see Figure 2). In the ankle, in a mild sprain, the ligament is only slightly stretched, and will usually fully recover. In a moderate sprain, the ligament is severely stretched and partially torn. It will usually heal but may be loose. In a severe sprain, the ligament stretches first, then completely tears. Usually, it is loose after healing. In a severe sprain, the cartilage can be injured as well.
About 80% of patients tear their ATFL, and the other 20% tear both the ATFL and the calcaneofibular ligament (CFL). The posterior talofibular ligament (PTFL) rarely is torn.
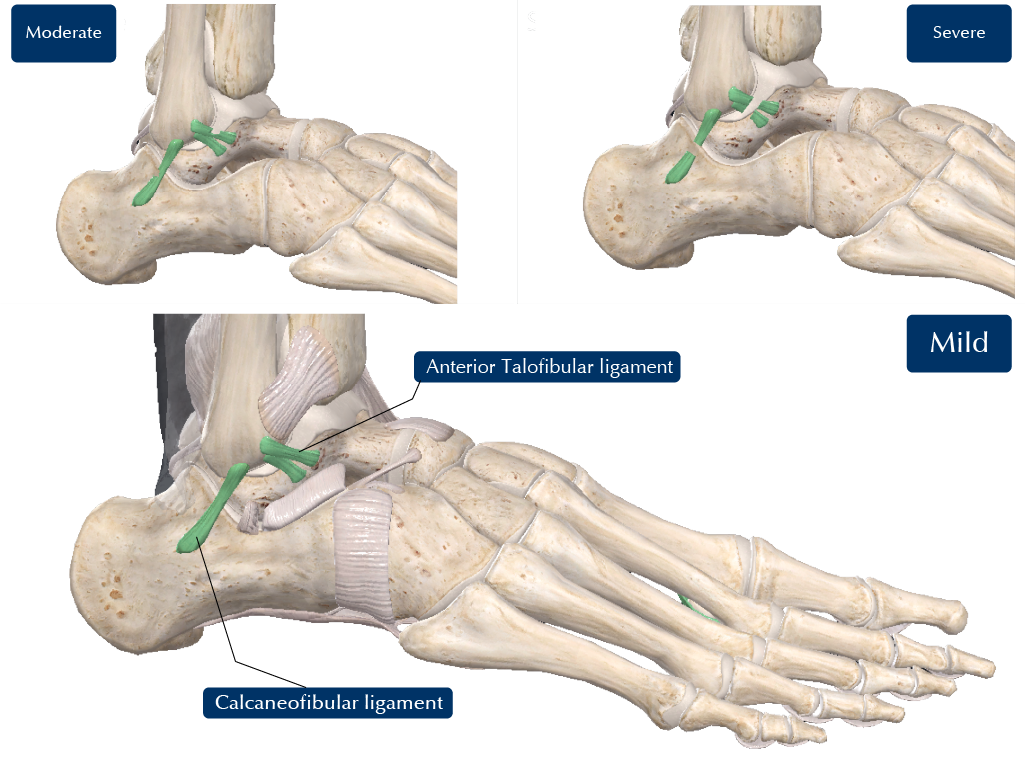 |
| Figure 2: Mild, Moderate and Severe Sprains. |
How does chronic ankle instability develop?
Chronic ankle instability typically follows on from an ankle sprain that did not heal properly.
How common are ankle sprains?
Common! An ankle sprain is one of the most common injuries in competitive athletes, especially in football, basketball, tennis and trail running. It also incurs in everyday life, simply walking or exercising on uneven surfaces, running across the road, or tripping on stairs.
How are ankle sprains treated?
Conventional wisdom recommends RICE (Rest, Ice, Compression and Elevation) and over-the-counter painkillers, followed by rehabilitation. Once the initial pain has settled, rehabilitation is important, to regain muscle strength and speed of reactions. Without good rehabilitation, there is an increased risk of developing ongoing ankle pain, arthritis and chronic ankle instability.
What are the symptoms of ankle instability?
- Ankle feels “weak” or “loose” or “gives out” or feels “unstable”.
- Pain, including aching and sudden catching or sharp pains
- Stiffness
- Swelling
Typically, an individual that has a moderate or severe ankle sprain stretches or completely tears one or two ankle ligaments. It is usually quite a significant event, the ankle is painful and swollen, and they are unable to play sport for a while. If the ligament does not sufficiently recover, the ankle gives way easily, and the ankle is repeatedly sprained, but, usually, these are not so sore, as the ankle ligament has already been torn, and is now loose, so it gives way without hurting the ligament again. Unfortunately, the cartilage gets injured, but, because the cartilage has no nerves, the damage may occur silently, so people may not realise how serious their ankle problem is. Eventually, spikes of new bone, called ‘osteophytes’ or 'bone spur', grow along the edges of the ankle joint, causing stiffness and pain (Figure 3).
 |
| Figure 3: X-ray of chronically unstable ankle showing osteophytes (green arrows) along the front of the joint. |
Is ankle instability serious?
Yes. Instability is a common cause of arthritis of the ankle (Figure 4). Ultimately the patient requiring ankle joint fusion (joining the bones together so the ankle is stiff, but painless) (Figure 5) or ankle joint replacement (with an artificial joint) (Figure 6).
 |
| Figure 4: X-ray of the ankle joint with arthritis, with loss of cartilage and osteophytes (arrows). |
 |
| Figure 5: X-ray of ankle joint fusion – the bones have been joined together with screws. |
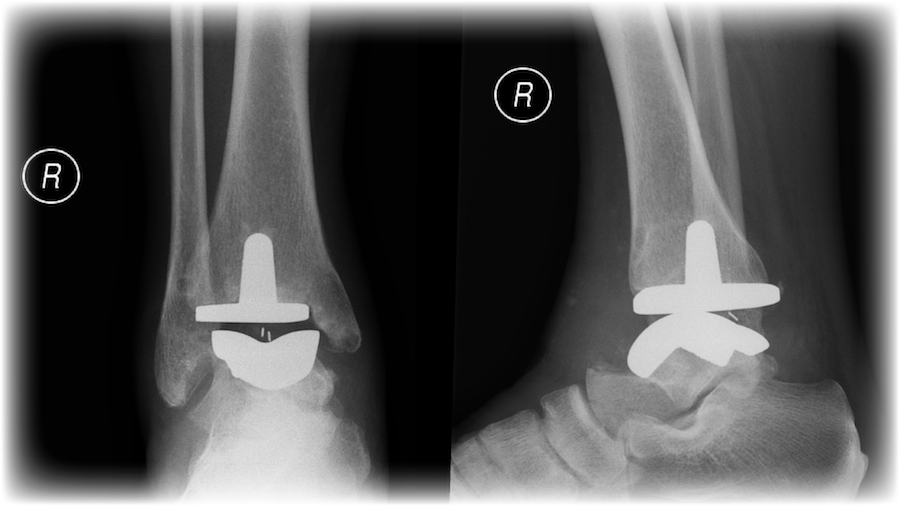 |
| Figure 6: X-ray of ankle joint replacement |
.
How is ankle instability diagnosed?
The seriousness of a severe ankle ligament injury can be overlooked by both individuals and medical professionals, as the problem is often relatively silent, and, initially, only slowly gets worse. There is often a combination of tightness of the joint and looseness of the injured ligaments, which can make it hard to work out what the problem really is.
Your doctor will physically examine your ankle looking for:
- Tenderness.
- Swelling.
- Ligament looseness.
- Impingement - pinching or jamming caused by osteophytes.
Are any tests useful?
X-rays
X-rays only show bones, and, in ankle instability, the injury is primarily to the ligaments, X-rays might appear normal even in a case of severe ankle instability, however the X-rays often demonstrate any ‘osteophytes’.
Stress X-rays
Taking an X-ray with the ligaments under tension can demonstrate abnormal movement in the ankle if the ligaments are injured. Originally the physician applied the stress by hand, wearing lead-lined gloves. Today we have special frames which apply a set amount of stress e.g. the Telos device (Figure 7). Comparison with the normal ankle (if there is one) is more accurate than only testing the injured side, because there are individual differences between patients. The Telos system is not widely used except by foot and ankle specialists. The design of the system enables correct anatomical positioning so that each ligament can be examined separately. The electronic display flags any muscular compensation, improving the accuracy of the examination. Figures 8 and 9 demonstrate an ankle which appears normal without stress, and the same ankle is clearly abnormal in a stress examination.
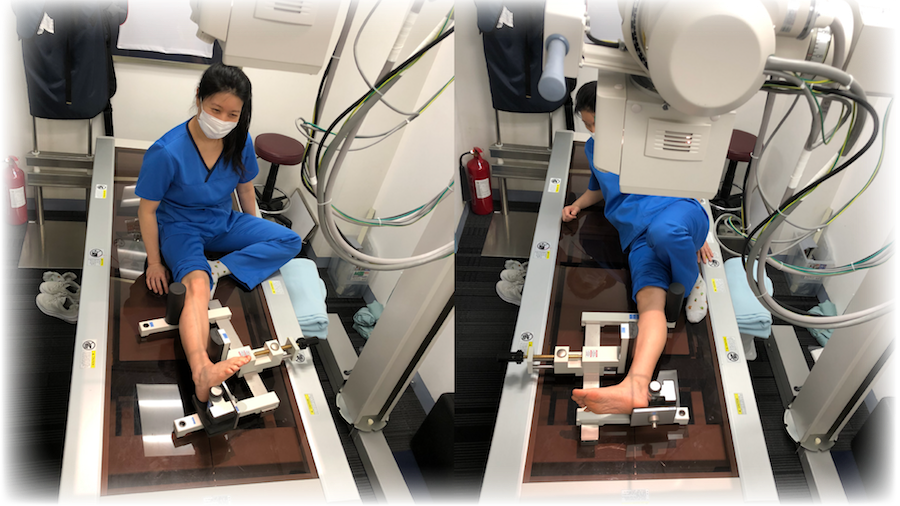 |
| Figure 7: Patients are positioned using Telos so their muscles are relaxed and stress is applied to different ligaments in different positions. |
The difference between X-rays and stress X-rays in an unstable ankle.
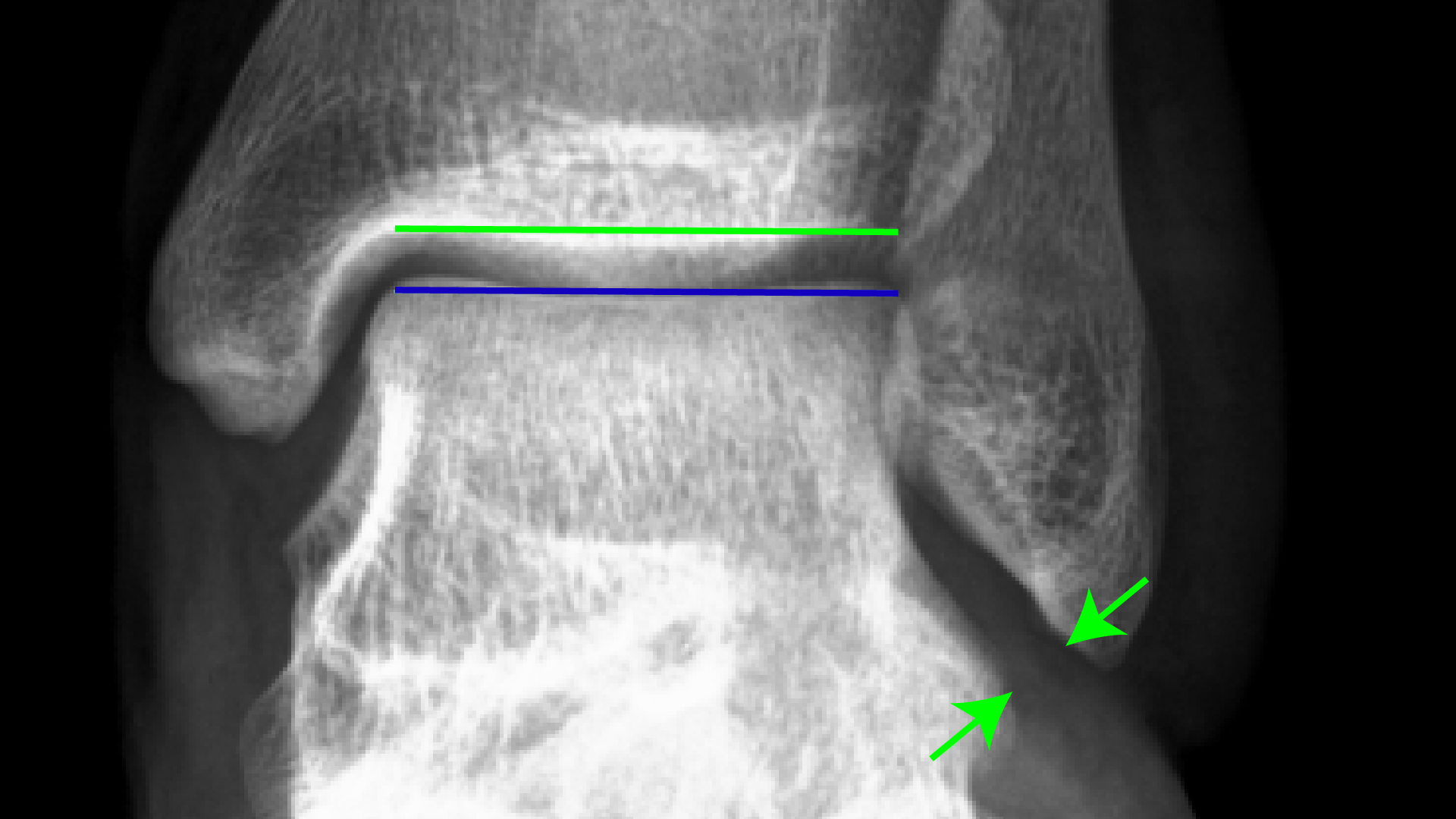 |
| Fig 8A: X-ray of the ankle appears normal when the joint is not under any stress: the ankle joint line as indicated by the green and blue lines is straight and parallel. The green arrows show the location of the ATFL. |
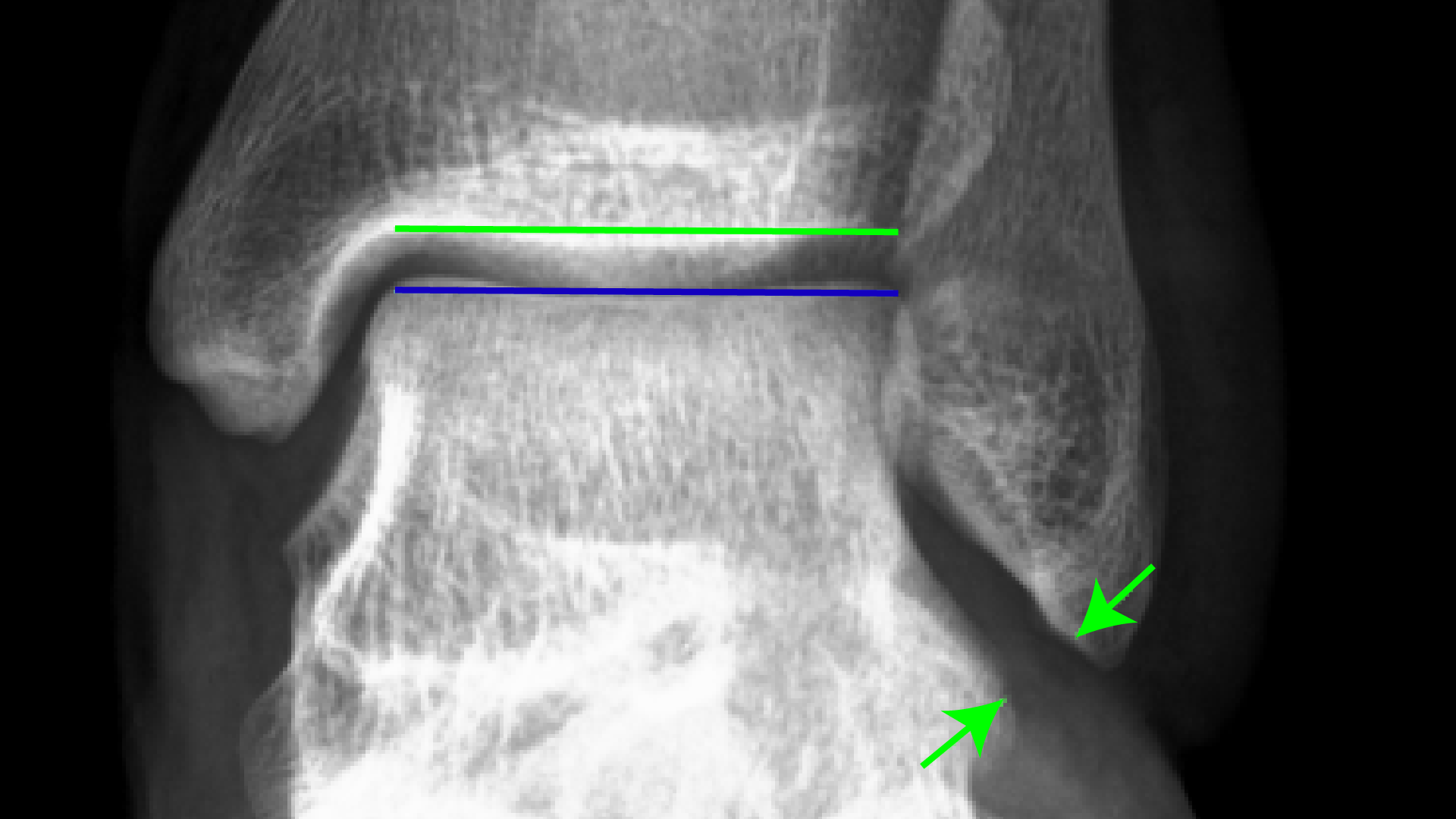 |
| Fig 8B: Under stress, the example joint is about 10º off parallel, and the gap between the arrows widens slightly, because the ligament is loose. |
Xray side view of the same ankle, showing instability when stress is applied to the joint.
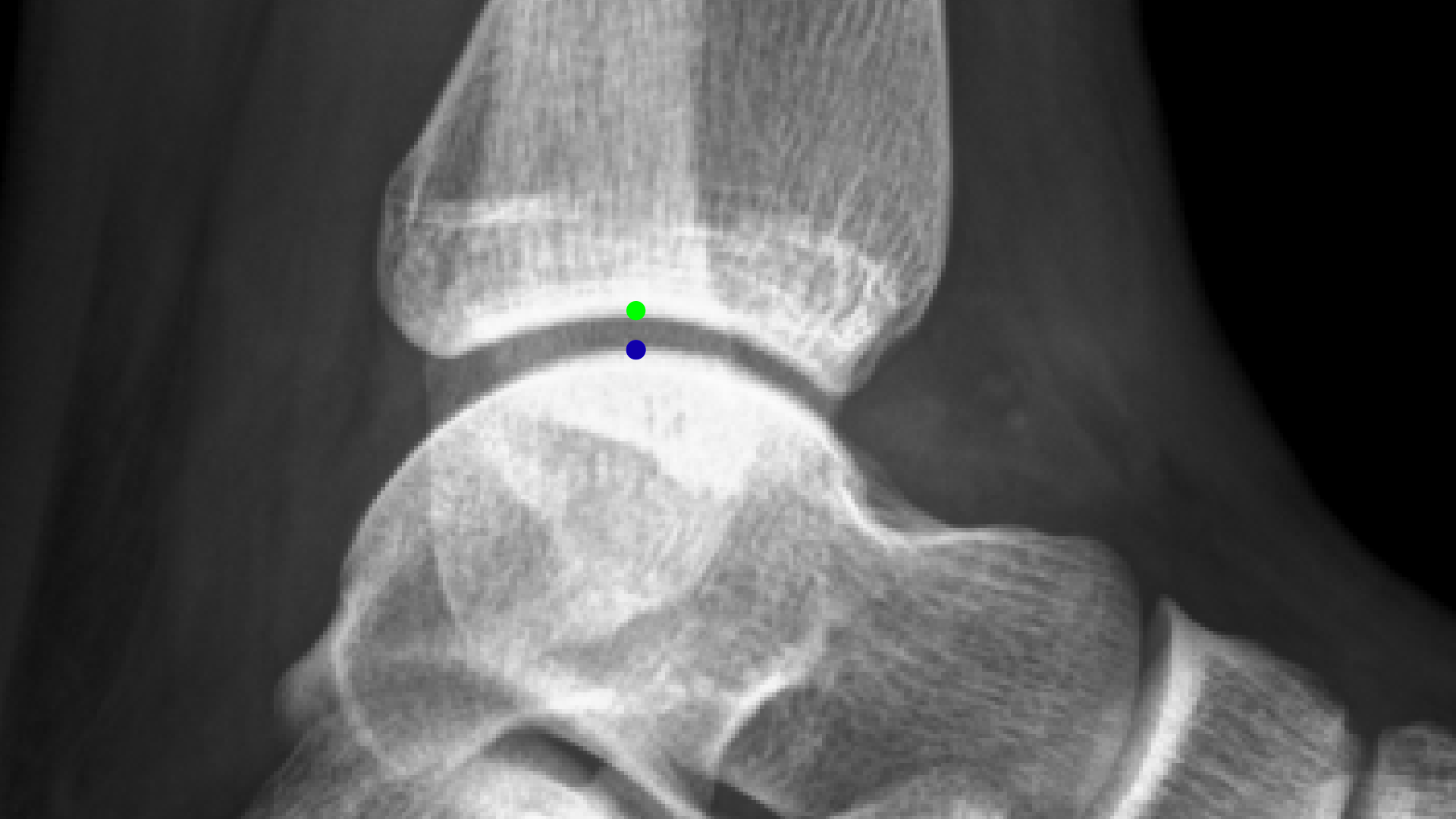 |
| Figure 9A: A regular X-ray from the side of the ankle without any stress - the green dot is the centre of the tibia (shin bone) and the blue dot is the centre of the talus (in the foot). |
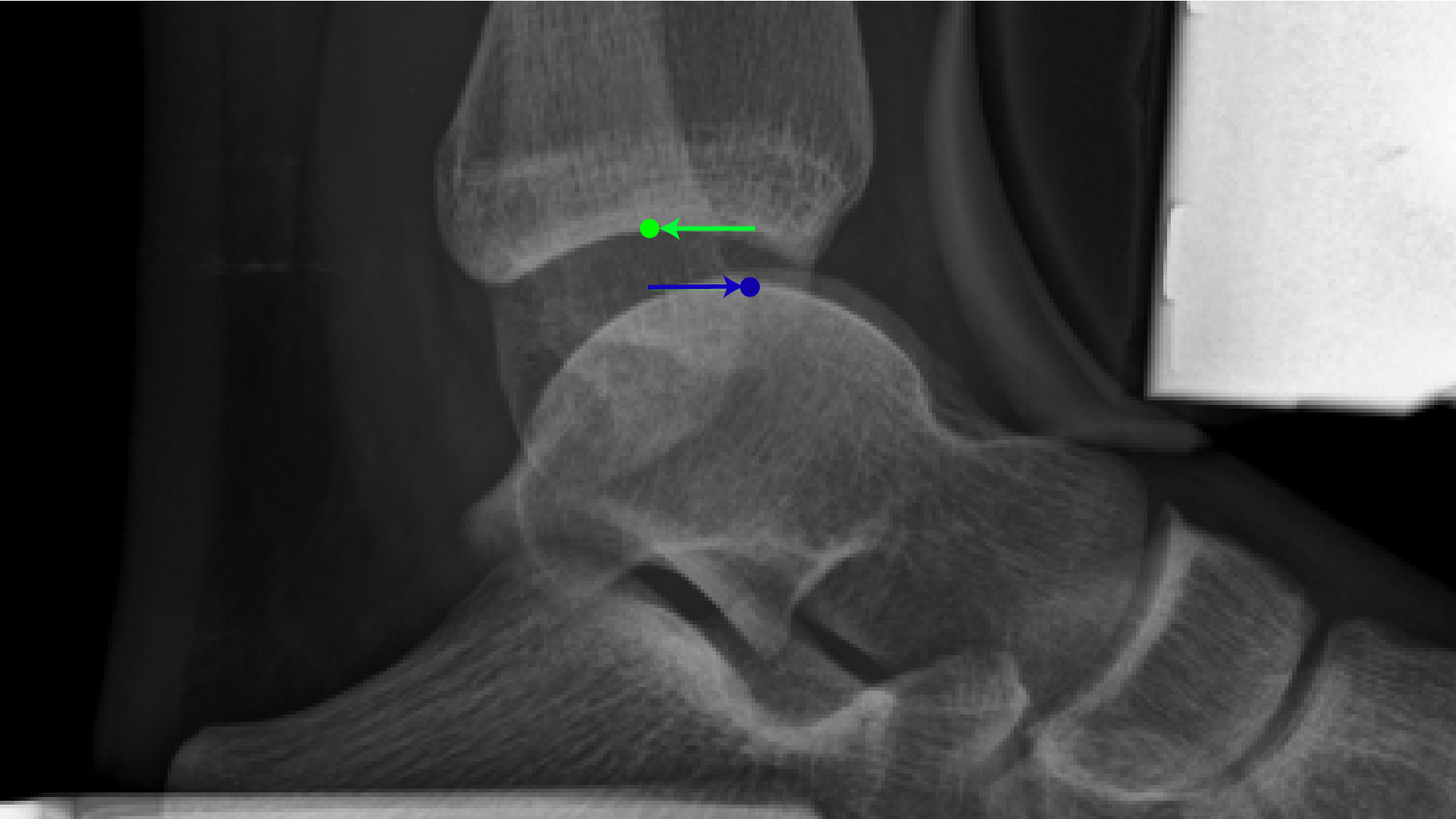 |
| Figure 9B: The stress X-ray – the foot is pushed forwards and the shin is pushed backwards. There is more than 1cm of movement, which is abnormal. |
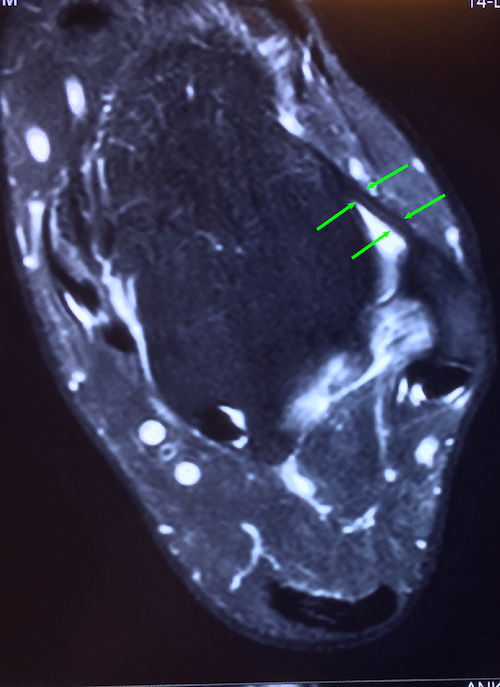 | 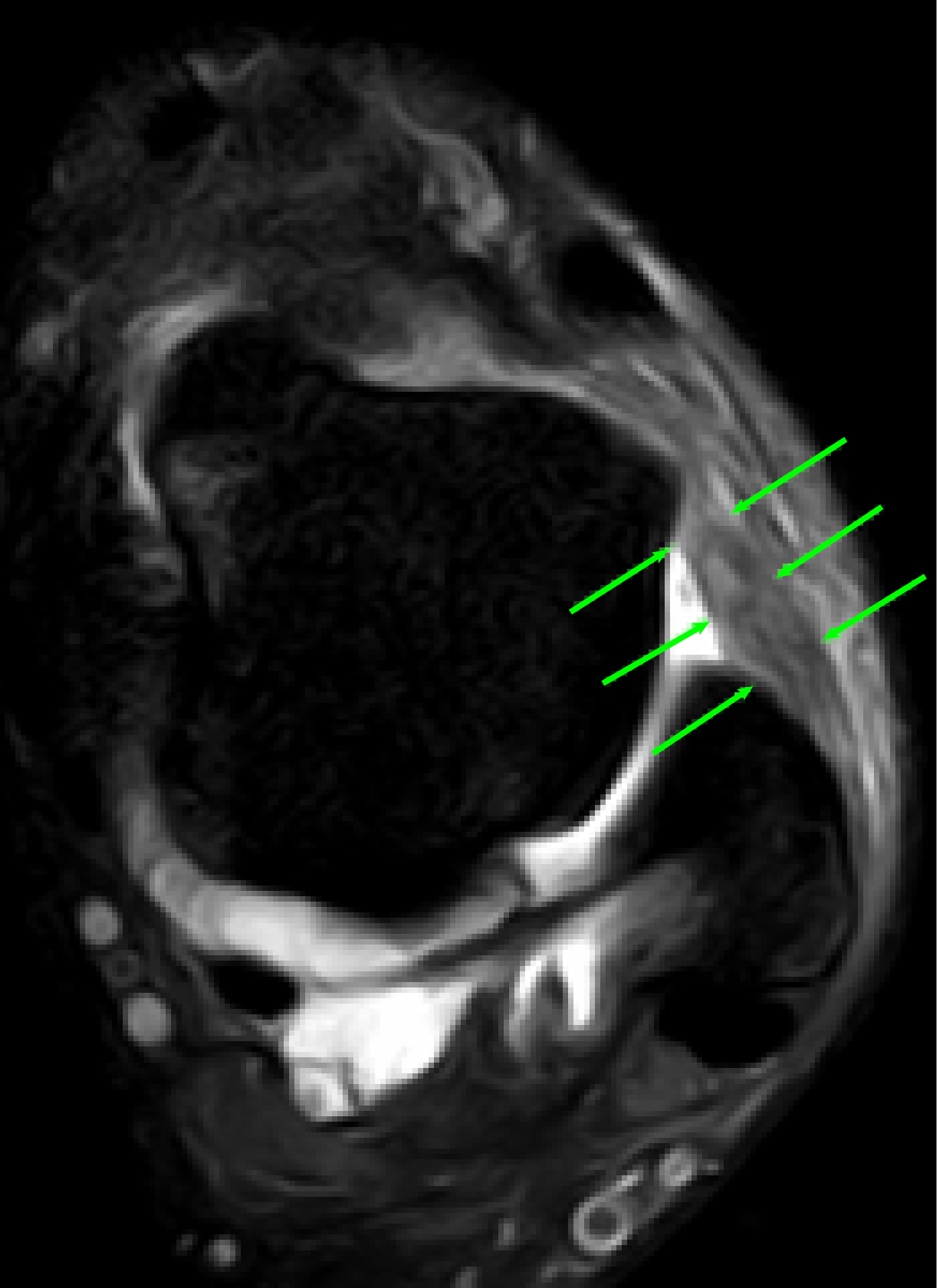 |
10A: Normal ankle: ATFL appears as a thin black line (arrows) 10B: Injured ATFL in the example unstable ankle appears as a thick wavy grey line (arrows). The white areas are fluid inside the ankle joint, signs of inflammation. | |
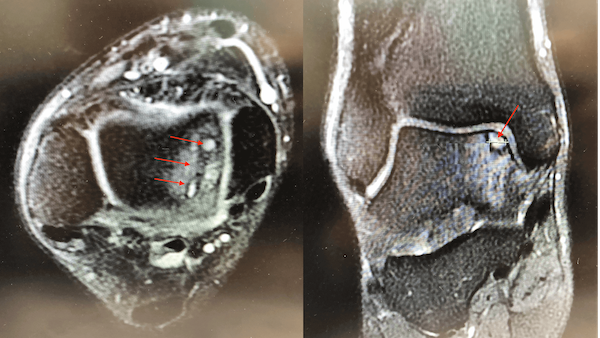 |
Figure 10C: RED arrows indicates cartilage damage in the ankle joint from chronic instability |
Magnetic Resonance Imaging (MRI)
An MRI scan demonstrate soft tissues as well as bone and can show fluid in the joint, bruising in the bone, and damage to cartilage as well as showing the ligaments.
Ultrasound scan
Can also be used to identify ligament injury.
What can be done about ankle instability?
Although a few people with severe instability might be offered immediate surgery, first-line treatment is generally non-surgical. Most people should undertake a physiotherapy programme tailored to their individual needs. Exercises and stretches are prescribed to increase strength and improve balance, range of motion, and reaction speed.
How long should non-surgical treatment last?
Physiotherapy is recommended for 6 weeks to 3 months, and maybe even as long as 6 months until the individual has managed to achieve optimum strength and stability.
Who needs an operation?
In about 10-30% of people, the ankle fails to recover with non-surgical treatment. Surgical treatment is recommended if there are continuing sprains, pain, difficulty with sport, or everyday activities.
What if I don’t want an operation?
Nobody wants an operation, but, if one has instability symptoms despite physiotherapy, there is a high risk of developing arthritis of the ankle, requiring ankle fusion or replacement later.
What does surgery involve?
The goal of surgery is to stabilise the ankle by repairing or reconstructing the damaged ligaments. Associated problems, such as impinging osteophytes and cartilage damage, can be treated at the same time.
Options are either conventional open surgery or new arthroscopic, “keyhole” surgery.
Essentially, the operations are the same, but open surgery, with a larger wound, has a slower recovery, so, if technically possible, arthroscopic surgery is preferred.
 |
Figure 11: Following arthroscopic ankle surgery, the two key-hole incisions are closed with a simple stitches leaving minimal scarring. |
How is the operation done?
The operation is done in an operation room in hospital. The patient has an anaesthetic – either general, ‘half body’ or regional (just the leg) so they cannot feel anything.
In an arthroscopic procedure, only two small incisions are needed, for a video camera and a set of tiny surgical instruments.
The photos (Figure 12) are taken by the video camera during an arthroscopic ligament repair procedure on our ‘example patient’. A small hole is drilled into the bone where the ATFL ligament has torn away; a ‘suture anchor’ is fixed in the bone; the suture is passed through the loose end of the ligament; and a knot is tied to reattach the ligament to the bone with the appropriate tension.
Local anaesthetic is injected into the ankle joint to reduce post-operative discomfort. The incisions are stitched closed. Waterproof dressings cover the incisions.
The patient can go home the next day, wearing a removable ‘cam walker’ boot (Figure 13).
Figure 12: Example ankle: arthroscopic surgical repair of the ATFL.
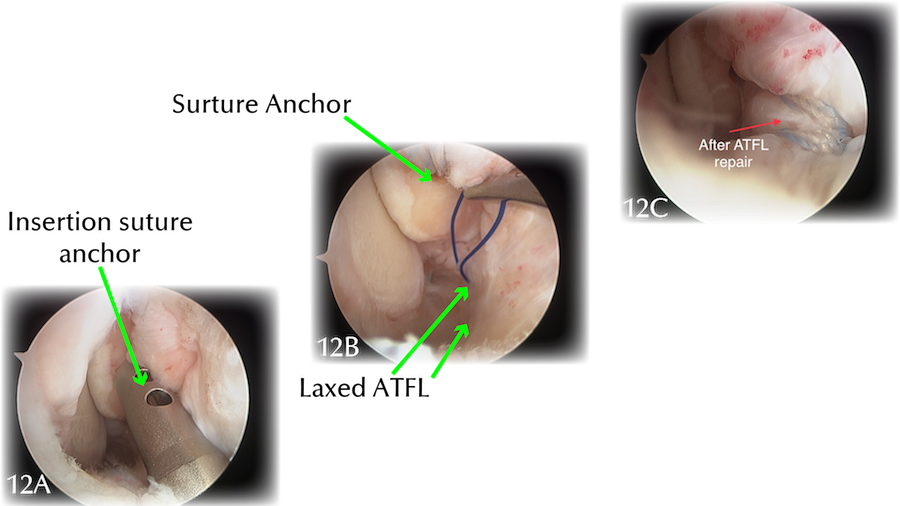 |
12A: Insertion of suture anchor inside a guide tube. |
What is the recovery?
Arthroscopic surgery enables a faster recovery time than open surgery. Usually the cam walker needs to be worn for 2-4 weeks (Figure 13) until one can walk better without it than with it. Using the walker appears to improve range of motion, as well as preserve muscle and bone mass compared with a traditional, immobilising cast.
One does a physiotherapy programme very similar to the pre-operation programme, as the goal is exactly the same: restoring strength; balance; range of motion; and reaction speed.
Most people return to jogging at 6 weeks; gentle sport after about 3 months; and are 90% recovered, playing contact sport, by 6 months.
 |
Figure 13: The removable cam walker is usually worn for 2-4 weeks. |
What is the long-term outcome?
The purpose of the above treatments are prevent ankle arthritis which may need ankle fusion or total ankle replacement.
References:
- Ferran NA, Oliva F, & Maffulli N. Ankle Instability. Sports Med Arthrosc Rev 2009;17(2):139-145.
- Galhoum AE, Wiewiorski M & Valderrabano, V. Ankle instability: Anatomy, mechanics, management and sequelae. Sports Orthop Traumatol, 2017;33:47-56.
- Golano P, Vega J, Perez-Carro L & Gotzens V. Ankle Anatomy for the Arthroscopist. Part I: The Portals. Foot Ankle Clin N Am. 2006; 11:253- 273.
- Guillo, S, Bauer T, Lee JW, Takao M, Kong SW, Stone JW, Mangone PG, Molloy A, Perera A, Pearce CJ, Michels F, Tourné Y, Ghorbani A & Calder J. Consensus in chronic ankle instability: aetiology, assessment, surgical indications and place for arthroscopy Orthop Traumatol Surg Res, 2013;(99S8), S411-S419.
- Hertel J & Corbett RO. An Updated Model of Chronic Ankle Instability. J Athl Train, 2019;54(6):572-588.
- Lee KM, Chung CY, Kwon SS, Chung MK, Won SH, Lee SY & Park MS. Relationship between stress ankle radiographs and injured ligaments on MRI. Skeletal Radiol. 2013; 42(11):1537–1542.
- Matsui K, Burgesson B,Takao M, Stone J, Guillo S, & Glazebrook M, ESSKA AFAS Ankle Instability Group. Minimally invasive surgical treatment for chronic ankle instability: a systematic review. Knee Surg Sports Traumatol Arthrosc, published online 11-2-2016
- Oakland Joint and Bone Specialists. Ankle Sprains. Oakland, California, United States. http://oaklandboneandjointspecialists.com/foot-ankle/ankle-sprains/ Accessed 1 May 2020.
- Ogilvie-Harris DJ, Gilbart MK & Chorney K. Chronic pain following ankle sprains in athletes: the role of arthroscopic surgery. Arthroscopy 1997;13(5): 564-574.
- Scheuba,G. Operating instructions telos-Stress Device GA-III/E. http://www.telosmedical.com/library/public/documents/PDFs/thelos-device.pdf Accessed 30 April 2020.
- Takao M, Matsui K, Stone JW, Glazebrook MA, Kennedy JG, Guillo S, Calder JD, & Karlsson J, Ankle Instability Group. Arthroscopic anterior talofibular ligament repair for lateral instability of the ankle Knee Surg Sports Traumatol Arthrosc, 2016;24(4):1003-1006.
- Myerson MS & Veljkovic A Eds. Managing instabilities of the foot and ankle. Foot and Ankle Clinics. 2018; 23(4). Elsevier. Philadelphia, Pennsylvania, United States.
