Femoro-Acetabular Impingement (FAI) FAQs
Femoro-Acetabular Impingement (FAI) FAQs
Written By Dr Jason BROCKWELL
(Last updated on: Oct 13th 2020)
What is this article?
This article is intended to give a general overview of the condition known as Femoro - Acetabular Impingement (FAI) for patients, their families and their family doctors and their physiotherapists.
What is Femoro – Acetabular Impingement?
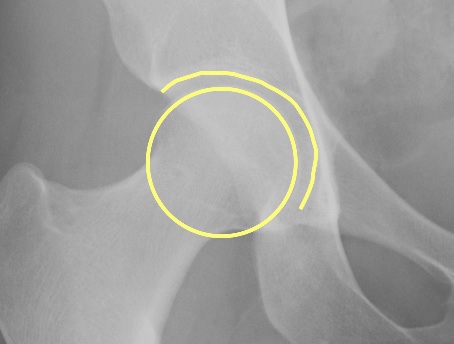
Femoro - Acetabular Impingement (FAI) is a condition in which the two bones which make up the hip joint pinch against each other, or 'impinge', at the extremes of motion, causing damage to the joint. (Fig. 1)
The hip joint is a ball and socket: the ball is formed by the head of the femur (thigh bone) and the socket is in the pelvis, and is known as the acetabulum, from its similarity (to early anatomists) to the shape of a Roman vinegar cruet. The gap between the two bones is filled with articular cartilage – the bearing surface of the joint – a smooth layer a few millimeters thick covers the bone on each side of the joint. (Fig. 2)
|
If the head of the femur is not round, or sits in the wrong position in relation to the rest of the femur, or the socket is either too deep or facing in the wrong direction, problems ensue. The most common form of FAI is 'primary' where the deformity does not follow a disease or injury, and is often quite subtle.
Primary FAI is a recently recognised condition.
Secondary FAI, where the impingement is clearly secondary to a disease, such as a slipped upper femoral epiphysis, or injury, such as a fracture, is well-known, and various operations have been described to correct it [1, 2].
Four types of primary FAI (Fig. 3):
1. Sports impingement
The hip is entirely normal, but extreme activities may damage the hip – for example repeated kicking in martial arts, lunging in racquet sports, the 'eggbeater' kick of water polo, kicking in soccer, horse riding etc. These activities push the hip to the extreme of its range of motion, and with repetition, the hip can be damaged.
Fig. 3 Four types of primary FAI: Normal, which can impinge in extreme positions in sport, thus the term ‘sports impingement’. The shaded area shows the ‘extra’ bone causing the impingement.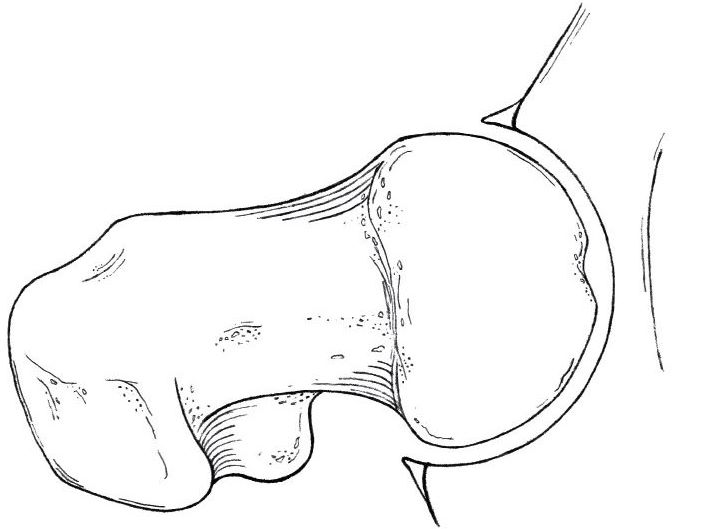 Sports impingement 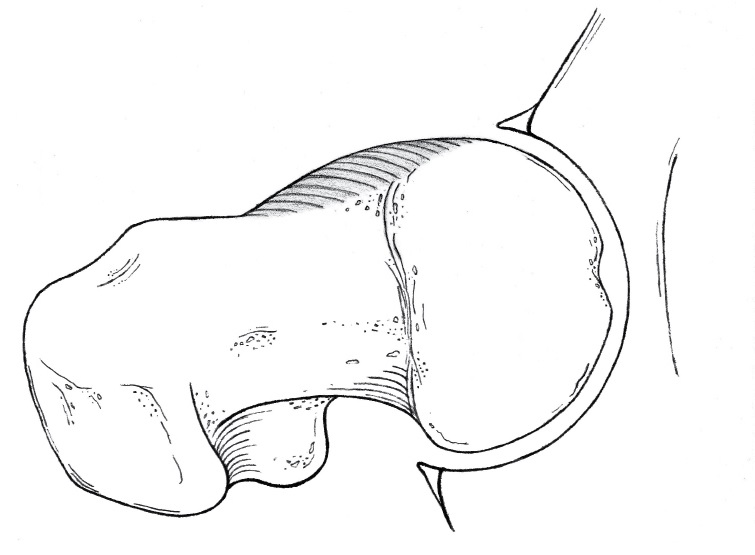 Cam 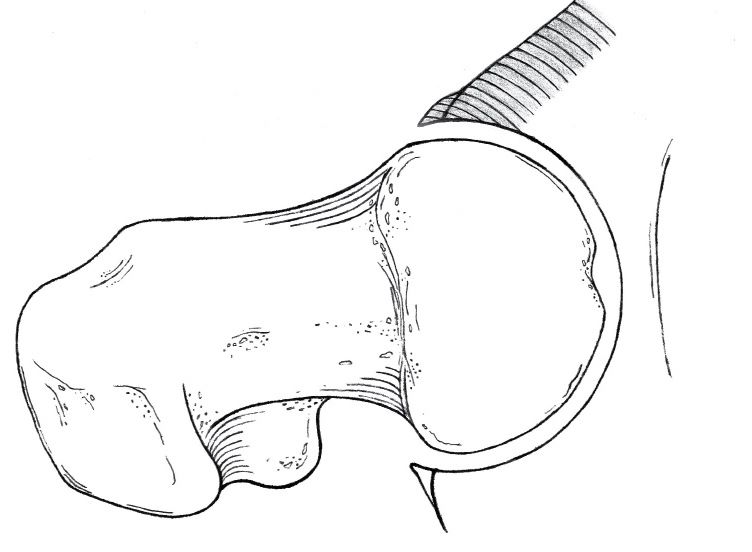 Pincer 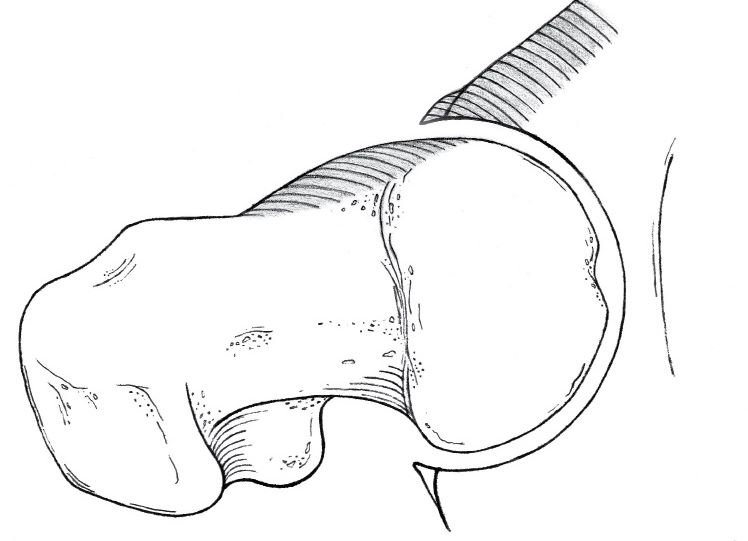 Mixed |
2. Cam impingement
This occurs most commonly in men. The femoral head is elliptical instead of round and the hip resembles a cam bearing rather than a roller bearing. (Fig. 4)
 Fig. 4 Cam shaft of an E-Type Jaguar car engine. The arrowheads show two of the cam lobes. |
The femoral head attempts to 'lift' the edge of the acetabulum, in the same way a cam shaft in a car engine lifts the valves. The effect is to strip the smooth articular cartilage off the acetabulum, causing arthritis. This might be compared to a door which has swelled in moist weather, and is now too big for the frame. As the door is repeatedly slammed to close, the plaster on the wall surrounding the door frames starts to fall off (analogous to the articular cartilage), followed by the frame breaking (an acetabular labral tear, similar to a meniscal cartilage tear in the knee), followed by the door failing to open or close properly at all (arthritis), and needing to be replaced.
3. Pincer impingement
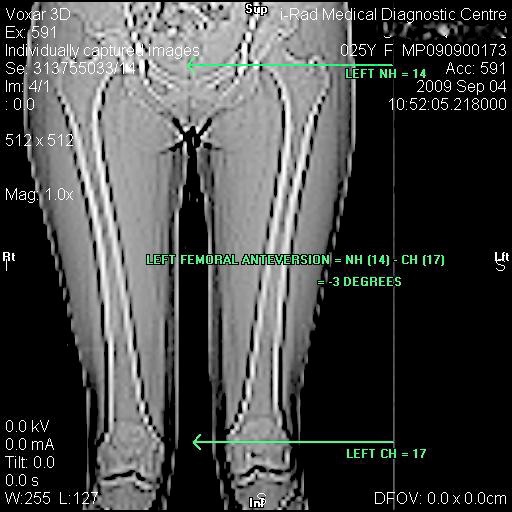
This occurs most commonly in women. Either the femoral anteversion is too little (the femur is not twisted in the correct way), or the acetabulum is too deep (coxa profunda) and/or facing backwards (retroverted). Jamming or 'pinching' of the acetabular labrum causes tearing of the labrum, and formation of extra bone – making the situation worse. It probably also causes articular cartilage damage leading to arthritis.
4. Mixed impingement
The most common problem is a mixture of cam and pincer impingement, though usually one form is predominant.
What is the natural history of FAI if left alone?
The natural history of primary FAI is uncertain, as the condition is only recently recognised, but it seems likely that FAI causes osteoarthritis (OA) of the hip joint because:
- FAI and OA hip are both common in Caucasians
- FAI causes damage to the articular cartilage of the hip, which most likely progresses to frank arthritis [3]
- Secondary FAI is well known to cause arthritis
How is FAI diagnosed?
'Primary' FAI is a recently-recognised condition, and many health professionals are not familiar with it, so the diagnosis is often delayed. X-rays may be reported as normal because they are not taken in the correct way to show FAI, or the signs of FAI may not be recognised. In addition there are many other causes of symptoms similar to those of FAI (essentially 'groin pain') which can make diagnosis difficult, even with adequate experience and appropriate investigations.
History: Most people complain of pain, which may be specifically felt around the hip, but more usually, the pain is nonspecific, and may be felt in the groin, buttock, sacro-iliac (SI) joint, low back, adductor muscles of the inner thigh or sometimes towards the knee. Sometimes painless FAI is identified in the asymptomatic opposite hip or when checking the hips of a person with knee problems.
Examination: Typically there is pain with Flexion, Adduction & Internal Rotation (the FADDIR test or anterior impingement test) of the hip. Often there is also discomfort and limited abduction in Flexion, Abduction and External Rotation (the FABER test). Sometimes there is a positive Drehmann's sign [4] - the hip runs into abduction and external rotation on flexion.
Investigations:
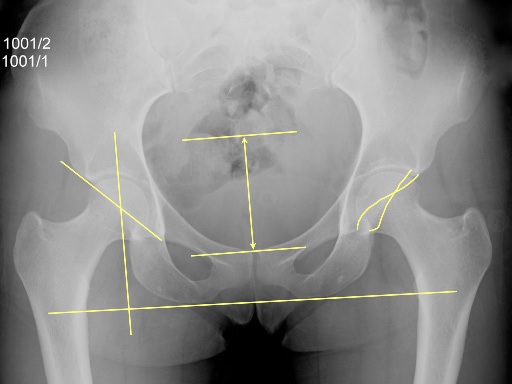
X-rays are usually diagnostic, if they are taken in the right way. The X-ray views needed to make the diagnosis are specially positioned supine AP pelvis & hips (Fig. 5) and true lateral or modified frog lateral views (Fig. 6) of both hips. X-rays of just one hip are not very useful, as there is no ‘horizon’ from which to measure angles – it is necessary to carefully position and X-ray the whole pelvis to begin to understand the anatomy of the hips.
|
Properly taken X-rays can show:
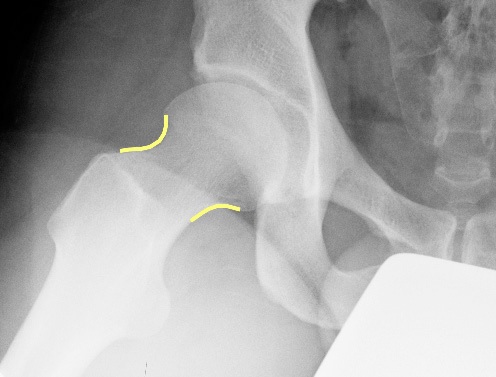
- The 'cam lesion' – extra bone on the femur giving the appearance of a 17th Century flintlock dueling pistol (Fig. 7) – thus known as a 'pistol grip deformity'.
 Fig. 7 17th Century flintlock dueling pistol – the rounded handle provides the name ‘pistol grip deformity’ to the characteristic X-ray appearance of a cam lesion. |
- The approximate shape of the acetabulum. By tracing the lines representing the front and back edges of the acetabulum it is possible to estimate the direction it faces, though this is only a guide, and CT or MRI is needed for accurate measurement.
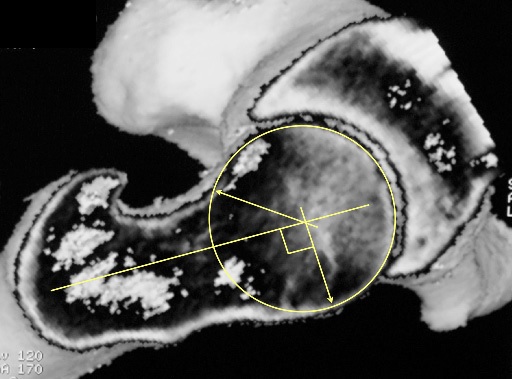
CT scan is very accurate for demonstrating the shape and positions of the bones (Fig. 8).
 Fig. 8 Three-dimensional reconstruction of a left hip made from CT scans. |
MRI will show other possible problems such as avascular necrosis of the femoral head (AVN), infection and tumour. Sometimes MRI can show damage to the articular cartilage, but, because the volume of the articular cartilage is quite small, it is hard to obtain good images. With improvements in MRI technology it should be possible to see more clearly (Fig. 9). The MRI must be performed according to a special protocol to be helpful.
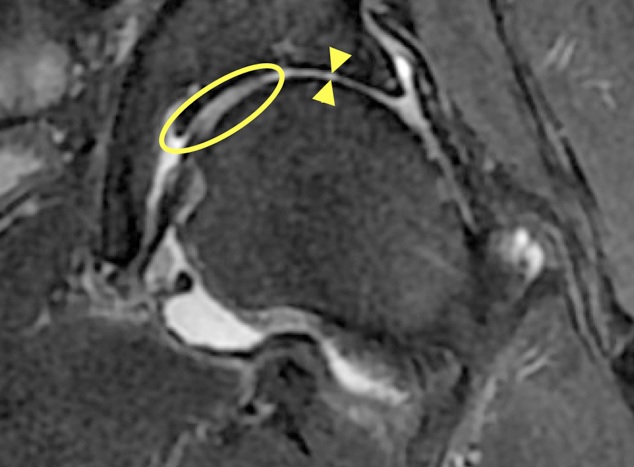 Fig. 9 MRI of the left hip. The bones are very dark grey. The medium grey area (circled) is normal articular cartilage. There is loss of articular cartilage in the superior part of the joint - the area between the arrowheads. |
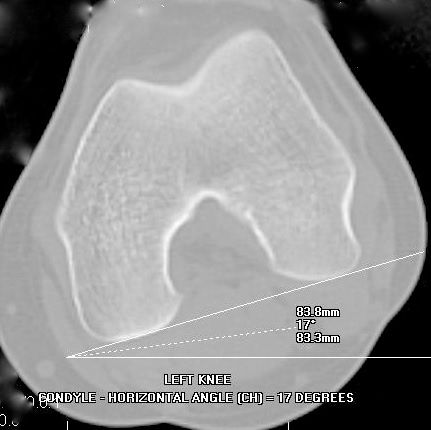
CT & MRI both allow measurement of the "alpha angle"[5] to quantify the cam impingement (Fig. 10), and measurement of the angles of the acetabulum and, important for full understanding of the problem, but often overlooked, the femoral version (Fig. 11). These scans must be performed according to special protocols to be helpful.
|
Injection: Injection of local anaesthetic +/- steroid +/- contrast into the hip joint may abolish pain, confirming the hip is the source of the pain.
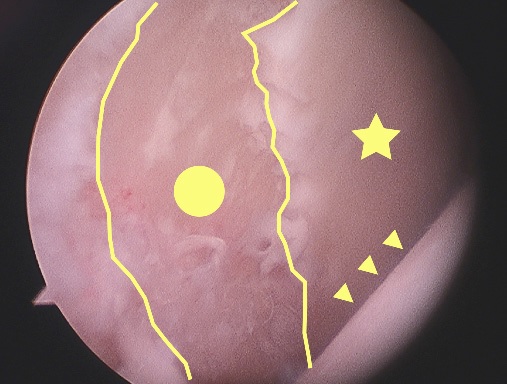
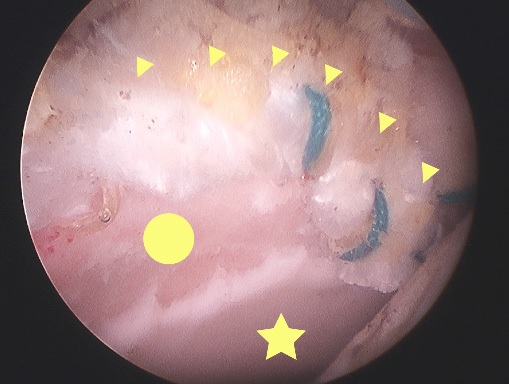
Arthroscopy: Characteristic damage is seen with the video arthroscope and the surgeon is able to probe the various structures inside the hip (Fig. 12A, B & C)
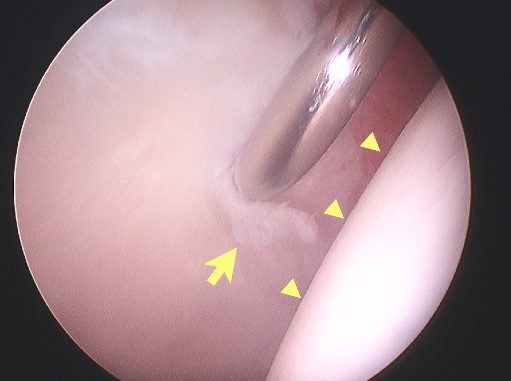 Fig. 12A Arthroscopic view of the hip of a skier. The probe is displacing damaged acetabular articular cartilage (arrow). The femoral head (arrowheads) is normal. 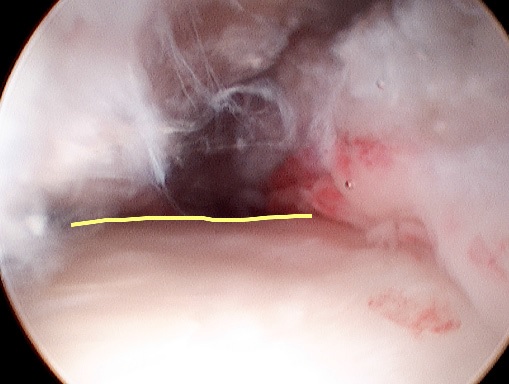 Fig. 12B Arthroscopic view of the head-neck junction in cam impingement – the flat appearance (yellow line) is clear. 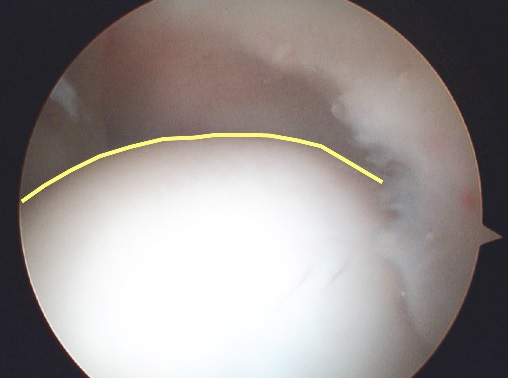 Fig. 12C Arthroscopic view of a normal head-neck junction – the round appearance (yellow line) is clear. |
Principal Differential Diagnoses (What else could it be?)
- Arthritis of the hip – most common in Caucasians.
- Avascular Necrosis (AVN) of the femoral head – where the bone dies because it does not have a sufficient blood supply. This is a particularly common problem in Asia.
- Acetabular dysplasia – where the acetabulum is too shallow, putting too much pressure on the articular cartilage. This is unusual worldwide, (especially as ultrasound screening programmes for newborn babies lead to earlier preventative treatment) but is more common in Caucasians and north Asians than south Asians.
- Other causes of hip pain - including infection, tumour, loose bodies, damage to the articular cartilage, synovitis, stress fracture of the femoral neck, transient osteoporosis of the hip.
- Other causes of groin pain - hernia, prostate, ovarian, from the back, from the sacro-iliac [SI] joint, stress fracture of the sacrum or pubis, adductor strain, osteitis pubis.
Treatment options
Mild cases
If the impingement is mild, and has been caused by an activity which can be avoided, simply avoiding the activity may be enough to settle the problem. Often a steroid injection helps to settle the inflammation in the hip joint.
Physiotherapy cannot correct the underlying problem of impingement, but it can relieve the painful muscle spasm associated with a painful hip joint, and it is helpful to discuss with a physiotherapist how to avoid impingement positions in daily life and in sport, and how to stretch and exercise without further harming the hip.
Moderate or severe cases
No treatment
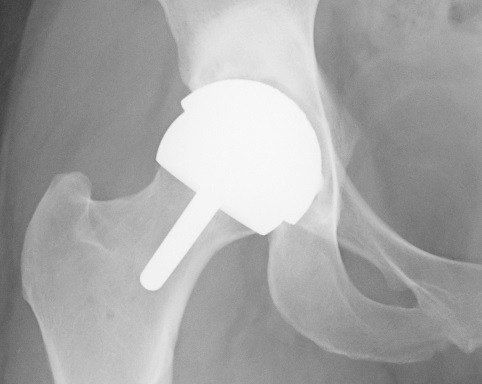
Avoid positions of impingement and accept likelihood of progression to arthritis. Modern joint replacements, such as the Birmingham Hip Resurfacing (BHR) (see www.birminghamhipresurfacing.com) can provide a near-normal hip.
Sports impingement
Arthroscopic (keyhole surgery) treatment of:
- articular cartilage damage, by debridement (leaving bare bone, which covers over with scar 1. tissue) (Fig. 13)
- any labral damage, by debridement, repair or reconstruction (Fig. 14)
|
Cam impingement
Arthroscopic or mini-open treatment of the femoral deformity by removing the extra bone on the femoral head-neck junction to restore the normal round shape of the femoral head (Fig. 15A & 15B)
|
Pincer impingement
Treatment depends on the cause and severity of the impingement.
Mild to moderate: Arthroscopic treatment of labral injury +/- articular cartilage damage plus arthroscopic acetabular rim recession (to make the socket less deep) or totally open surgical treatment by surgical hip dislocation.
Severe impingement: May require femoral rotation osteotomy (cutting and correcting the twisting of the femur) or acetabular realignment osteotomy (cutting the bones of the pelvis and repositioning the acetabulum).
Mixed impingement
Combination as above.
What are the results of treatment?
Because FAI is relatively recently recognised, there are no long-term outcome studies. There are good medium-term results for treatment by 'open' surgery – dislocating the hip, reshaping the bones to correct the impingement, and replacing the hip, and there are good short-term outcomes from arthroscopic treatment [6].
The key factors for good results are:
1. Catching the problem early enough, before there is severe articular cartilage damage – articular cartilage does not heal, so, although it is possible to reduce further damage by removing the impingement, it is not possible to 'turn back the clock'.
2. Completely correcting the impingement, by whatever means are necessary – for example, in some cases arthroscopy is insufficient and an osteotomy is required.
How urgent is arthroscopic treatment?
It is very hard to say, but, if one has pain, one already has significant damage, and, given that the arthroscopy can only prevent further damage, not undo damage already-done, it is better to have the procedure as soon as reasonably possible – usually within 3 months.
How bad can my hip be and still be helped by arthroscopy?
Again It is very hard to say, but, if one has 3mm or less of articular cartilage on the X-ray (Fig. 16A), or if one has 'central osteophytes' (extra bits of bone separate from the impingement osteophytes) it is probably too late. In dubious cases MRI may help, but there are technical limits to the accuracy of MRI. Sometimes there appears to be a good layer of articular cartilage, but, at arthroscopy, it is falling off the acetabular bone like loose ceiling tiles.
In doubtful cases one may have to decide to go ahead with either arthroscopy or hip replacement (Fig. 16B) based on very limited information and one's personal feeling about what is right for one's self (see below).
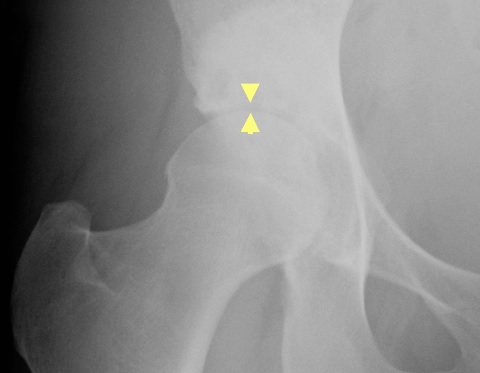
Fig. 16A Narrow joint space (the gap between the tips of the arrowheads).
|
What if it is too late – can I have a hip replacement?
If one is too late for hip arthroscopy to be helpful, either because the X-ray or MRI shows severe articular cartilage damage, or, at arthroscopy, the articular cartilage that was hoped to be in good condition is actually falling off the bone of the acetabulum like loose ceiling tiles, one could have a hip replacement.
For the young and active population group considered for hip arthroscopy, a special hip replacement is required, such as a Birmingham Hip Resurfacing.
This could be performed:
- instead of a hip arthroscopy
- at the same procedure if the arthroscopy showed severe damage
- later, if it was agreed to see the effect of the hip arthroscopy before having a hip replacement.
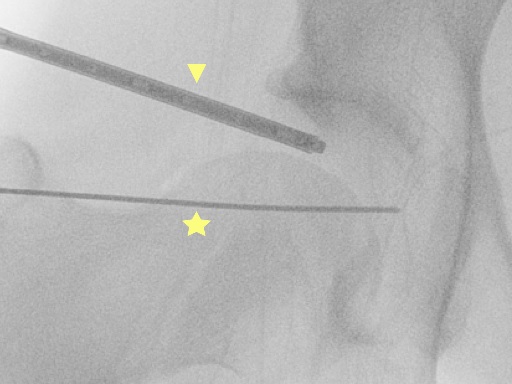
How is hip arthroscopy performed?
This is explained in detail in the document 'Asia Medical Specialists Hip Arthroscopy Patient Information'. Briefly: 24 hours in hospital; general anaesthetic; 2 small holes in the top of the thigh; small instruments are passed into the hip joint under X-ray image intensifier guidance (Fig. 17); the procedure is performed using video images from the arthroscope; the hip is 'sore' but not 'painful' afterwards; one can walk immediately with the aid of crutches; one leaves hospital the next day; dressings are waterproof, so one can shower normally; one can return to an office job after 2 – 3 days; one uses crutches for 3 weeks; one can return to sports training after 3 months.
|
What are the risks of hip arthroscopy?
As with all surgical procedures there are risks, but hip arthroscopy is pretty safe – it is very unusual to actually make someone worse by means of a hip arthroscopy, and the vast majority of people feel better. This document is intended as a general overview of FAI and is not intended to be comprehensive. For patients who are actually considering a hip arthroscopy, the risks (and all the other issues) are covered in detail in the document ‘Asia Medical Specialists Hip Arthroscopy Patient Information’.
My other hip looks the same on the X-ray, but does not hurt – should I have a prophylactic arthroscopy?
Because we do not know the natural history if primary FAI, we cannot say whether hips with certain X-ray appearances will go on to develop arthritis, therefore we are unable to recommend preventative treatment, and only recommend operating on painful hips. If one were to have an arthroscopy on a painless hip, and it were to become painful afterwards, possibly as a result of a complication, one would be pretty upset!
Where can I get more information?
If you are considering a hip arthroscopy with Asia Medical Specialists, please read the document 'Asia Medical Specialists Hip Arthroscopy Patient Information' which is available from Asia Medical Specialists. (Reading this is part of the consent process for the procedure.)
If you would like to review the scientific literature on FAI go to www.pubmed.gov and enter 'femoro-acetabular impingement' into the search box.
Do I really need an injection? But I don't like needles!
Injection of local anaesthetic +/- steroid +/- contrast into the hip joint may abolish pain, confirming the hip is the source of the pain. Sometimes it can take the pain away permanently.
The injection goes into the front of the upper thigh, and is not particularly uncomfortable. There is only one injection, usually containing a mixture of drugs, and it only takes a few seconds. It is more uncomfortable than a flu shot, but actually far worse in prospect than in practice. Many people are quite nervous about the injection, but then surprised (and relieved!) by how quick and painless it is.
- Usually the local anaesthetic works within a few minutes, significantly improving the pain.
- The local anaesthetic only lasts a few hours. The steroid works for up to about 3 weeks.
- The steroid does not have much effect for a day or two, so sometimes the hip is more sore, as a result of the injection, later on the day of the injection, or the day after. If this occurs it is helpful to take an anti-inflammatory tablet such as ibuprofen (Nurofen; Brufen; Advil).
- The steroid mostly stays inside the hip joint and does not affect the rest of the body significantly, but enough gets into the rest of the system for diabetics to notice that their blood sugar control is worse than normal for a few days or longer. Sometimes the diabetic control is quite significantly affected.
- There are no significant long-lasting effects from a single steroid injection. Repeated injections may damage • the articular cartilage, hastening arthritis.
- The major risk of the injection is the introduction of bacteria into the hip joint and infection of the joint. This is extremely rare.
- The other risk is an allergic reaction to one of the drugs. The local anaesthetic is lignocaine (Lidocaine; Xylocaine) and is commonly used by dentists. If you have never had problems with a reaction to a dental local anaesthetic, it is very unlikely you will react to a hip injection. It is extremely unusual to react to a steroid, as steroids are used to treat allergic reactions, but it is possible to have a reaction to a preservative or other chemical in the mixture.
- The injection is usually performed 'freehand' - judging the correct position by reference to the bones of the • hip and pelvis. Occasionally it is difficult to judge the correct position, and it is helpful to inject some X-ray contrast in with the other drugs and take an X-ray to confirm the injection is inside the joint (or not!) or to perform the injection under ultrasound guidance.
- Sometimes the injection does not have any effect on the pain. The likely reasons for this are:
The cause of the pain is not the hip joint.
The injection is not in the hip joint.
The injection is in the hip joint, but local anaesthetic has got 'stuck' in one part of the joint and cannot spread around to anaesthetise the joint.
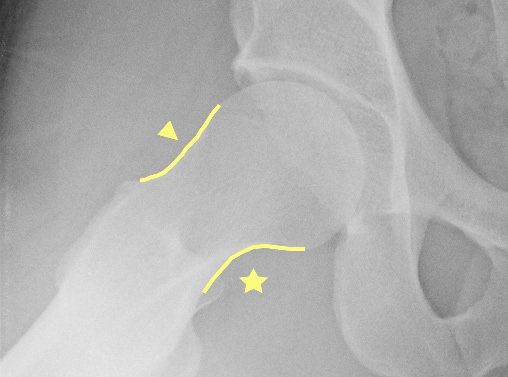
In these cases it is best to wait for about a week to see if the steroid relieves the pain. If there is no effect, it is worth repeating the injection possibly with X-ray (Fig. 18) or ultrasound guidance, to confirm the location. If the injection is confirmed to be inside the joint, but has no effect on the pain, one should consider non-hip joint problems as the cause of the pain.
 Fig. 18 X-ray shows white contrast inside the hip joint (arrowheads) and the thin injection needle (arrow). |
X-ray technique for femoro-acetabular impingement
Two specially positioned X-rays are required. In fact one is a ‘standard’ view, and the other is a slight modification of a standard view, so no special equipment or expertise is required.
X-ray number 1: AP pelvis & hips. This is a 'standard' X-ray of the whole pelvis and hips taken with the subject lying down. The legs are internally rotated 20 degrees to make the femoral necks parallel to the plane of the film. The beam is centred at the pubic symphysis at the level of the tips of the greater trochanters of the femora. The beam to film distance is 1 to 2 metres.
On the film, one should check that the pelvis is not:
1. rotated - by seeing that the sacral spinous processes and the pubic symphysis, which are both in the midline, line up.
2. flexed or extended - by seeing that the tip of the sacrum is within 2 to 5 cm of the superior pubic rami.
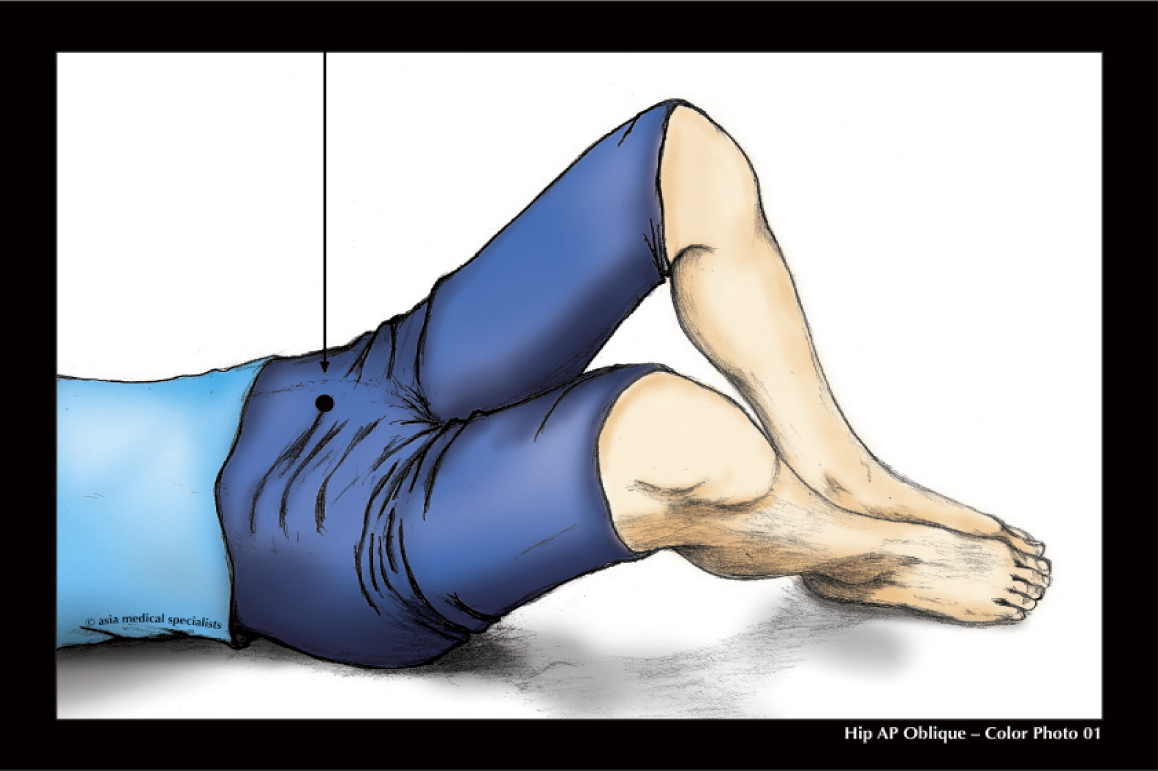
X-ray number 2: Modified frog laterals both hips. This is a slight modification of the standard frog lateral in that the hips are not abducted (ie the legs spread apart) as much. The subject lies supine and the beam is centred in the same way as for the first X-ray, but the legs are bent up at the hips and the knees bent to 90 degrees. (Fig. 19A&B)
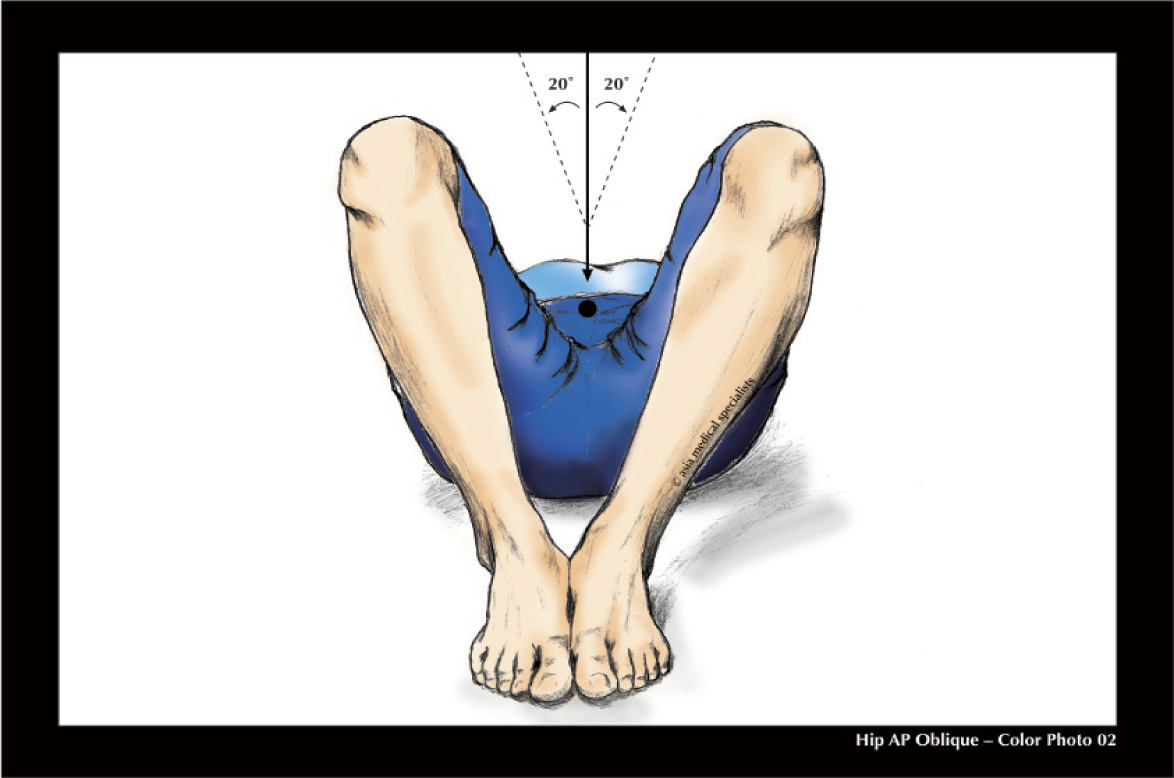
The feet are placed next to each other, with the soles flat on the table, and the legs are spread slightly (abducted 20 degrees from the vertical, for a total arc between the thighs of 40 degrees). (Fig. 19B)
Fig. 19A Modified frog lateral X-ray: the beam is centred on the public symphysis.
|
On the film, one should check that the pelvis is not rotated by seeing that the sacral spinous processes and the pubic symphysis, which are both in the midline, line up, but the pelvis is expected to be flexed in this position.
GlossaryAcetabulum: Socket of the hip joint. |
References
1. Heyman, C.H. and C.H. Herndon, Slipped Femoral Epiphysis with Severe Displacement: A Conservative Operative Treatmenmt. J 1. Bone Joint Surg Am, 1957. 39(2): p. 293-413.
2. Smith-Petersen, M.N., TREATMENT OF MALUM COXAE SENILIS, OLD SLIPPED UPPER FEMORAL EPIPHYSIS, INTRAPELVIC 2. PROTRUSION OF THE ACETABULUM, AND COXA PLANA BY MEANS OF ACETABULOPLASTY. J Bone Joint Surg Am, 1936. 18(4): p. 869-880.
3. Beck, M., et al., Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br, 2005. 87(7): p. 1012-8.
4. Drehmann, F., [Drehmann’s sign. A clinical examination method in epiphysiolysis (slipping of the upper femoral epiphysis). Description 4. of signs, aetiopathogenetic considerations, clinical experience (author’s transl)]. Z Orthop Ihre Grenzgeb, 1979. 117(3): p. 333-44.
5. Notzli, H.P., et al., The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint 5. Surg Br, 2002. 84-B(4): p.556-560.
6. Philippon, M.J., et al., Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral 6. dysfunction: MINIMUM TWO-YEAR FOLLOW-UP. J Bone Joint Surg Br, 2009. 91-B(1): p.16-23.
| Copyright ©2017 Asia Medical Specialists Limited. All rights reserved. |