Articular Cartilage Injuries in the Knee: FAQs
Articular Cartilage Injuries in the Knee: FAQs
written/reviewed by doctors of Asia Medical Specialists
(Last updated on: Oct 13th 2020)
What is articular cartilage?
Fig. 1A Knee with area of cartilage damage on the thigh bone (arrow). |
Fig. 1B Cross section through the injury shows the layer of articular cartilage on the thigh bone, with an area of injury (arrow). The black triangles are the meniscal cartilages. |
How is articular cartilage injured?
These injuries are more common in children than adults, probably because children have relatively thick cartilage and weak bone.
How are articular cartilage injuries diagnosed?
On examination, typically there is not much to find unless there are other injuries or a fresh are of damage is within reach of the examiner's touch.
X-rays
Fig. 2 Knee joint surgically opened reveals a large area of bare bone (arrow) where a |
MRI
What is the 'natural history' of an articular cartilage injury?
- sharp edges to round off (Fig. 3);
- loose fragments of cartilage floating around in the joint to either be resorbed or to grow larger as they are nourished by the synovial lubricant fluid;
- exposed bone 'heals' by forming scar tissue (composed of fibrocartilage, which, while better than nothing, does not have the same mechanical properties of articular cartilage).
|
Treatment
Non-operative treatment includes physical therapy to optimise muscle strengthen and balance, soft-soled shoes to absorb impact, avoiding impact, taking glucosamine, and ‘viscosupplementation’ – the injection of lubricants into the joint as explained in the OA Knee FAQs.
There are several options:
1. Repairing the loose pieces of cartilage or cartilage and bone
2. Removing loose fragments or free-floating 'loose bodies'
3. 'Microfracture'
4. 'Osteochondral grafting'
5. 'Autologous chondrocyte implantation'
6. Salvage type surgery, such as osteotomy or joint replacement
Repair
Removing loose fragments or free-floating 'loose bodies'.
Removing loose fragments of cartilage so the edges of any crater are clean (Fig. 4), and removing 'loose bodies', which are floating around in the joint, may significantly improve pain and mechanical symptoms, even though the 'clean' crater will not 'heal'. This procedure can usually be performed arthroscopically.
Fig. 4 The rough edges and base of the 'crater' have been cleaned up. |
Fig. 5A Microfracture seen at arthroscopy – there are small holes in the pink bone, some of which are bleeding. |
Fig. 5B Diagrammatically, the holes are placed in the base of the 'crater'. |
Microfracture
'Microfracture' is the technique of making little holes in the bone in the base of a cartilage crater to cause bleeding. The bleeding encourages ‘healing’ by the formation of scar fibrocartilage, which can be thought of as scar tissue (Fig. 5). The surgery is short, minimal invasive and with a quick recovery. It is the most frequently used cartilage procedure [1] and seem to result in significant functional improvement [2,3], however there are very few controlled trial, i.e. comparing microfracture to other forms of treatment.
Osteochondral grafts
The original technique was to take a cylindrical ‘plug’ of bone and cartilage from a less important part of the knee and tamp it into a same sized hole made in the injured area (Fig. 6) like placing tiles in a mosaic, hence the alternative name ‘mosaicplasty’. Because bone heals well, this is a successful procedure, but the drawback is that the cartilage in less important areas of the knee is thinner than in the weight-bearing areas (which are usually the ones which cause symptoms when injured, and thus need this kind of advanced treatment).
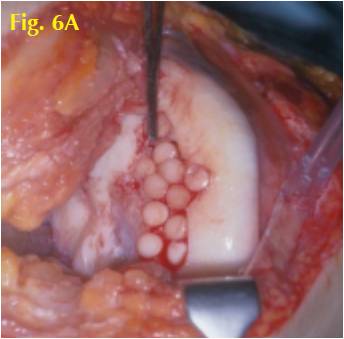 Fig. 6A Intraoperative view of osteochondral grafts placed in the knee. |
Fig. 6B Diagrammatically: The grafts are taken from less important areas (yellow arrow) and placed in the damaged area (blue arrow). |
The donor site fills up with fibrocartilage, and the chondrocyte and osteocytes in the graft survive [4].
Indications include primary treatment of small to medium sized injuries in relatively high-demand patients. It is advantageous by virtue of using the patient's own tissue and eliminating immunological concerns. It is limited by the size of the graft. The major risk is plug failure and donor site problems. Post-operative rehabilitation includes yearly range of motion and non-weight bearing for 2 weeks, with an increase to full-weight bearing from 2-6 weeks. The results have been favourable with intermediate-term follow-up [5,6]. Studies in athletes under the age of 40 has shown significant superiority over microfracture, with a higher chance of return to sports at the pre-injury level [7].
With the success of this technique, surgeons have also performed 'allografts' where tissue is taken from a donor, and synthetic grafts, where a synthetic material acts as a 'scaffold' for the patients own cells to grow on. These procedures have the advantages of no donor site problems, but the disadvantage that they do not bring in living articular cartilage cells.
Autologous Chondrocyte Implantation
Autologous chondrocyte implantation (ACI) is a very appealing treatment because it brings new cartilage cells to help heal the injury, but it involves two operations, and it is quite expensive. It is a two-stage procedure beginning with biopsy of normal cartilage from the non-weight bearing area (Fig. 7). The cartilage cells are then cultured in a special laboratory, where they multiply until there are enough to repair the damage. At a second procedure they are implanted into the defect. The result is 'articular-like' cartilage which is biomechanically superior to fibrocartilage.
|
|
ACI is often used as a secondary procedure (because of the inconvenience and cost) for the treatment of medium to large cartilage injuries in young patients with high physical demands. Results in appropriate cases are >85% good and excellent. Micheli et al 8 reported superior results with ACI when the procedure is performed early after the onset of cartilage pathology and poor results with delayed treatment. It suggests that the remaining articular cartilage is damaged by abnormal loading over time [9,10,11].
The latest 'third generation' technique is called 'matrix-induced autologous chondrocyte implantation' (MACI) (Fig. 8). The cartilage cells grow on a protein sheet, which can be rolled up and delivered into the joint arthroscopically, allowing the technique to be used in areas of the joint which are not accessible by other means.
|
References
1. Cartilage repair approach and treatment characteristics across the knee joint: a European survey. Salzmann GM, Niemeyer P, Steinwachs M, Kreuz PC, Sudkamp NP, Mayr HO. Arch Orthop Trauma Surg. 2011 Mar;131(3):283-91.
2. The microfracture technique for the treatment of articular cartilage lesions in the knee: A prospective cohort study. Kai Mithoefer, Riley Williams, Rusell F. Warren, Hollis G. Potter, Christopher R Spock, Edward C. Jones, Thomas L. Wickiewicz, Robery G. Marx. J Bone Joint Surg Am, 2005 Sep 01:87(9):1911-1920.
3. Microfracture for treatment of knee cartilage defects in children and adolescents. Salzmann GM, Sah BR, Schmal H, Niemeyer P, Sudkamp NP. Pediatr Rep. 2012 Apr 2;4(2):e21.
4. Arthroscopic osteochondral transplantation: Histological results. Barber FA, Chow JC. Arthroscopy. 2001 Oct;17(8):832-5.
5. Autologous osteochondral mosaicplasty for the treatment of full thickness defects of weight bearing joints:10 years of experients and clinical experience. Hangody L, Fules P. J Bone Joint Surg Am. 2003;85(supple):25-32
6. 10-year follow-up of a prospective, randomized clinical study of Mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint of athletes. Gudas R, Gidaite A, Pocius A, Gudiene A, Cekanauskas E, Monastyrekiene E, Basevicius A. Am J Sports Med. 2012 Sep 28.
7. A prospective randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint in young athletes. Gudas R, Kalesinskas RJ, Kimtys V, Stankevicius E, Toliusis V, Bernotavicius G, Smailys A. Arthroscopy. 2005 Sep;21(9):1066-75.
8. Autologous chondrocyte implantation of the knee: multi-centre experience and minimum 3-year follow-up. Micheli LJ, Browne JE, Erggelet C. Clin J Sport Med. 2001;11:223-228.
9. Transplantation of cartilage-like tissue made by tissue engineering in the treatment of cartilage defects of the knee. Ochi M, Uchio Y, Kawasaki K, Iwasa J. J Bone Joint Surg Br. 2002;84:571-578.
10. Autologous chondrocyte transplantation: Biomechanics and long term durability. Peterson L, Brittberg M. Am J sports Med. 2002;30:2-12.
| Copyright ©2017 Asia Medical Specialists Limited. All rights reserved. |
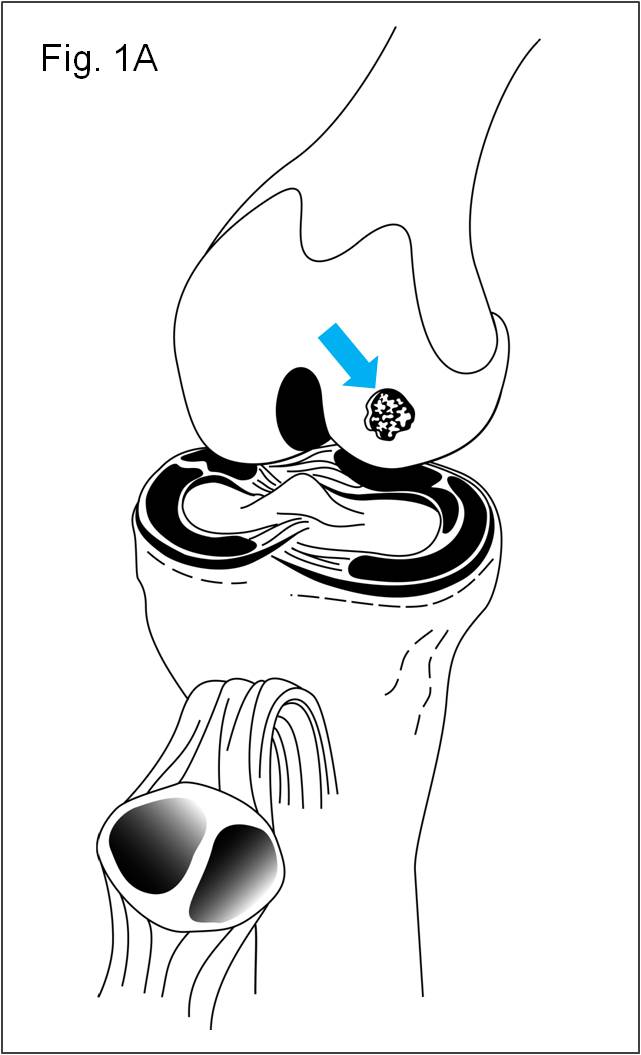
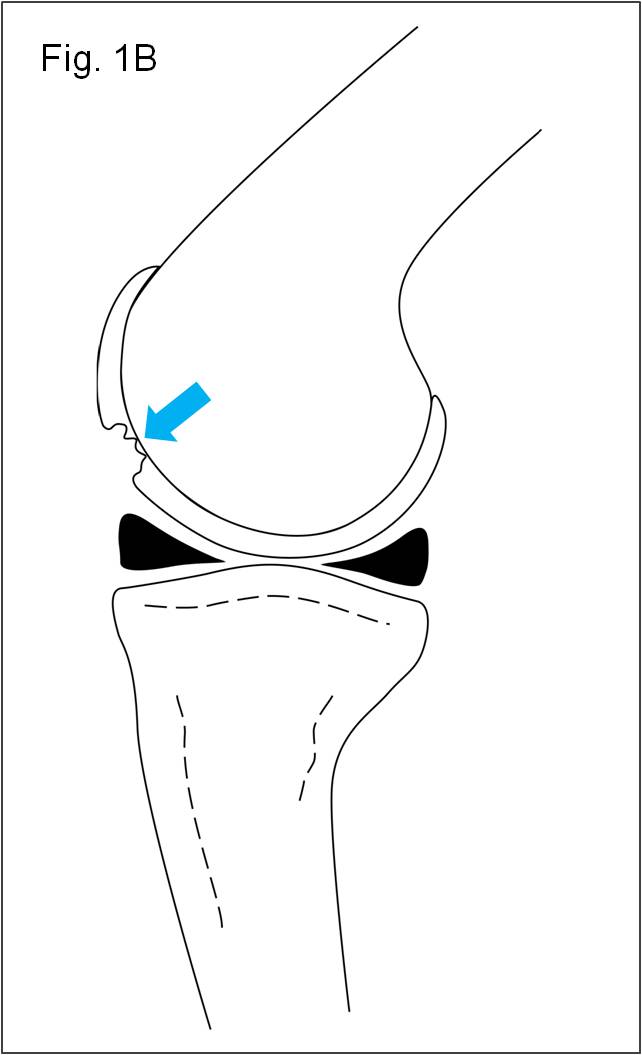
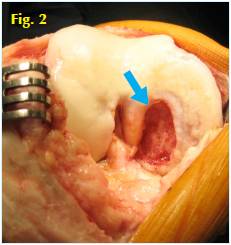
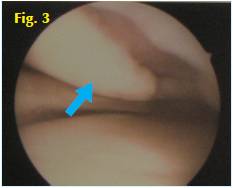
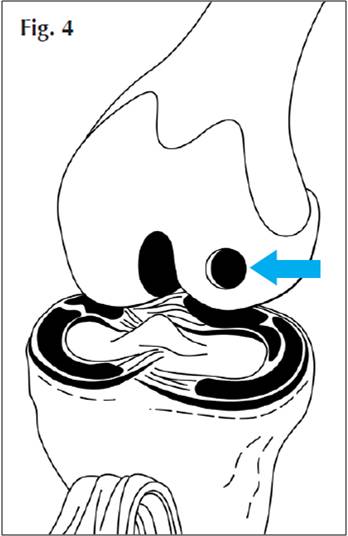

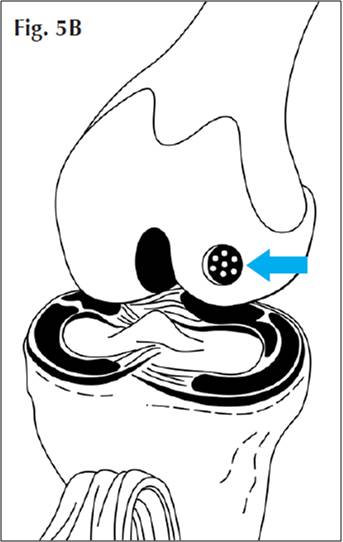
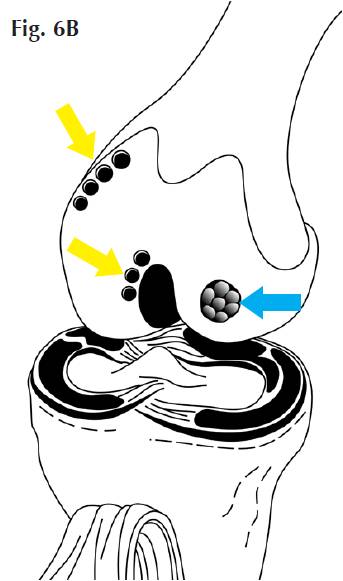
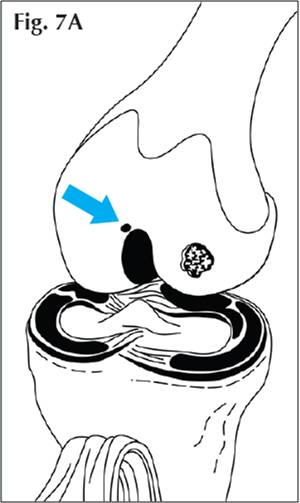
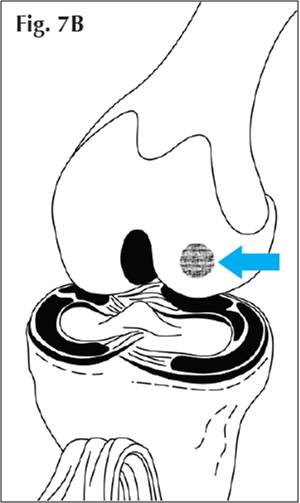
 Fig. 8 Matrix-induced Autologous Chondrocyte Implantation (MACI). The pale pink membrane is being glued into place in the knee.
Fig. 8 Matrix-induced Autologous Chondrocyte Implantation (MACI). The pale pink membrane is being glued into place in the knee.