Choosing Among Different Types of Hip Replacement FAQs
Choosing Among Different Types of Hip Replacement FAQs
Written By Dr Jason BROCKWELL
(Last updated on: Oct 13th 2020)
What are the alternatives to hip replacement for arthritis of the hip?
First line treatment:
1. Physiotherapy to learn ‘joint protection’.
2. Swimming or cycling each morning to ‘loosen up’ the hip.
3. Soft soled shoes and avoiding impact.
4. Diet rich in Omega 3 (essentially a fish diet – OK for people who enjoy fish and do not enjoy red meat, but probably not worthwhile for steak lovers).
5. Glucosamine 1.5 grams once per day regularly [1, 2].
6. Paracetamol/acetaminophen [Tylenol or Panadol] as required for pain. If pain is not controlled by paracetamol one can take anti-inflammatories such as ibuprofen (Advil/Nuroen/Brufen) diclofenac (Voltaren) or etoricoxib as needed.
Second line treatment: Injections of steroid, platelet rich plasma (PRP) or hyaluronic acid as required.
Third line treatment: Therapeutic arthroscopy (keyhole surgery) if the arthritis is not too advanced. This option is worth considering if there is over 2mm of joint space on the X-ray, especially for younger people.
Final: Hip Replacement surgeries.
When should I consider hip replacement surgery?
We believe that modern hip replacement surgeries will last for many years, so there is little advantage in delaying the procedure if pain is affecting sleep or daily life despite treatments outlined above.
What kind of hip replacement surgeries are available?
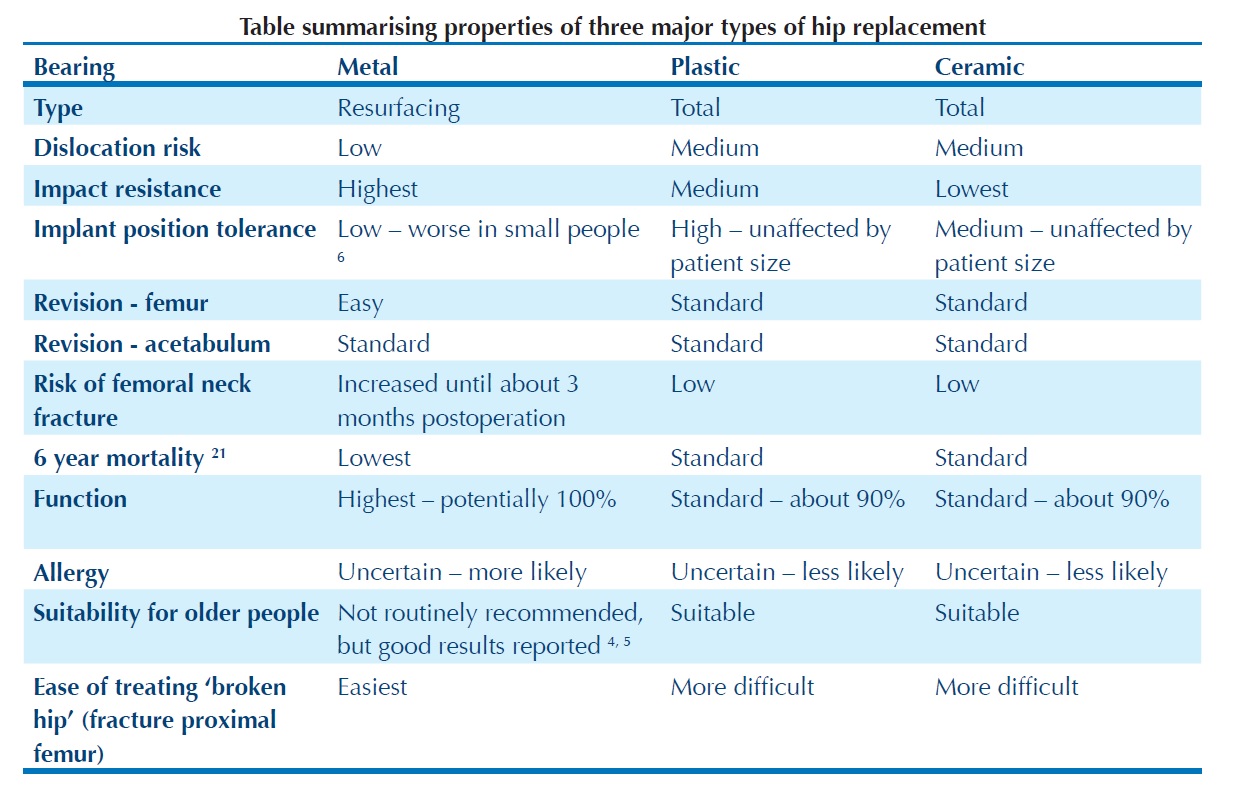
There is a variety of modern total hip replacements which would give a good result, and three major modern bearing combinations: metal or ceramic on cross-linked polyethylene; ceramic on ceramic and metal on metal.
How long do they last?
The most important issue affecting the longevity of a total hip replacement is wear particles generated by the bearing. The early designs of metal on polyethylene (developed by Sir John Charnley) functioned well in the medium term, but all failed in the longer term because the wear particles caused a reaction which led the the bone supporting the implant to be eaten away.
New bearings have been devloped to overcome this problem. Of those commonly available today, all are giving good medium term results, but none has been in use long enough for us to see the long term results.
The original polyethylene bearings have been treated with radiation to cross-link the molecules in the polyethylene (similar to vulcanising rubber) and improve wear resistance. However the bearing is not lubricated, and some wear particles are generated, in proportion to the amount of activity of the patient. We believe that a modern polyethylene bearing will take 20 years to generate enough wear debris to loosen the implant with moderate use – for example a person of average weight who is not especially active.
Ceramic bearings have been developed which produce less total quantity of wear debris, although higher numbers of particles, because the individual particles are smaller, but they seem to be less biologically active, and cause less bone reaction. Like polyethylene bearings, most modern ceramic bearings are not fully lubricated, but they do require some lubrication, and ceramic bearings can squeak if they do not get adequate lubrication, but they have excellent longevity, and may last for life.
Metal bearings are, when correctly positioned, fully lubricated, and do not produce any significant wear, however, if they are poorly positioned they produce very corrosive wear debris which eats away the tissues very quickly. Some of the early metal bearings, implanted in the 1960s, outlived their owners, so it is possible that a lubricated metal bearing could last indefinitely.
What about activity?
Metal bearings offer the best chance of the highest possible functional recovery, as the bearings are not brittle (unlike ceramics) and can therefore withstand impact, and, because of their large diameter, very rarely dislocate (unlike smaller diameter polyethylene and ceramic bearings), so one can return to unrestricted activity.
What about other factors?
There are, of course, other factors to consider, but for most individuals, the other factors are relatively minor after longevity and activity.
Should I choose a hip resurfacing or a conventional total hip replacement surgery?
If you are a young man with osteoarthritis, there is little doubt that you are best with a hip resurfacing. Resurfacing was designed for young men with osteoarthritis, and the Australian National Joint Replacement Registry reports that for men under 55 years of age with osteoarthritis, the Birmingham Hip Resurfacing is the best performing of
all kinds of hip replacements in Australia [3]. If you are older or female, the question is more difficult to answer.
I am older – what should I choose?
Although hip resurfacing was developed for the specific problem of young active people wearing out conventional hip replacements, hip resurfacing is not limited to young people only. Governments making health care decisions for their entire populations will not recommend hip resurfacing for older people, as the additional cost of the resurfacing implant (versus cheaper conventional THR implants) is not worth it from a public health point of view. Also, the additional technical challenge of performing a resurfacing versus a conventional THR means that slightly fewer will be performed in the same amount of time.
However, for an individual in good health, who aspires to be more active than the average individual of the same age (Heli-skiing versus shopping), there is no evidence that resurfacing carries more risk (maybe because the trials have not been carried out) and there are reports of good success in older people [4, 5]. My oldest patient was 88 when he had both of his hips resurfaced in one operation. He was soon back on the golf course, and is very happy. Slightly younger patients (in their sixties & seventies) put their resurfacings to good use – hiking, swimming, golfing, skiing, cycling etc.
Could they have done this with conventional THRs? Possibly. Golfer Tom Watson famously played off for the British Open 9 months after a conventional THR, but he is unusual. Jack Nicklaus has not played competitively since his conventional hip replacement.
I am female – what should I choose?
There is some concern that women do relatively poorly with resurfacings, and there is conflicting evidence, but there is a substantial body of opinion that, controlled for implant size, there is no sex difference, in other words, men and women of the same size do equally well 6. That said, smaller people do not do as well as larger people, probably because there is less room for error in acetabular cup positioning with smaller sized implants. Recently, several manufacturers of resurfacings have stopped making the smaller sizes, effectively restricting resurfacing to patients about 5’7” and taller. Smith & Nephew, the manufacturers of the Birmingham Hip Resurfacing do not
recommend its use in women at all - however this position is very controversial.
What gives better function? Hip resurfacing or conventional THR?
As with most things in medicine, there is much debate, but much recent evidence supports the position that hip resurfacings give better function [7-10].
However there are at least two papers which report no difference [11, 12]. One of these papers was criticised for reporting a difference of 10% in walking speed as ‘no different’ when many would argue that the ability to walk 10% faster is very significant [13], however the other paper describes a well-designed trial, so there is at least one study reporting no difference in function.
As far as I am aware, there are no reports of worse functional outcomes in hip resurfacing compared to conventional THR.
What if I have osteoporosis?
In general, osteoporosis is not a problem. In individuals with osteopaenia or osteoporosis of the neck of the femur, the bone density recovers after hip resurfacing [14, 15]. In conventional THR the neck of the femur is removed and replaced with metal, so bone strength is not a big issue.
What if I ‘break my hip’?
The term ‘broken hip’ usually applies to older people breaking the upper end of their femur (thigh bone) as a result of a fall. Young people can break their hips, but, as the bone becomes weaker because of age-related decreases in bone density (osteoporosis), this injury is more common in older people. It is a serious injury. If one has a hip replacement of some sort, one can still break one’s hip – but the bone breaks around the hip replacement. If one has a hip resurfacing the broken hip follows the same pattern as in a natural hip, and is treated in the same way [16-19]. If one has a total hip replacement the bone breaks around the femoral stem, and is more difficult to treat [20].
This is not yet considered to be an important factor in choice of hip replacement design, probably because hip replacement surgeons do not deal with many broken hips, but, as the younger patients who are receiving hip resurfacings grow older and suffer ‘broken hips’ in larger numbers, it is likely that the trauma surgeons who deal with the majority of broken hips will compare the outcomes, and I expect they will conclude that patients with resurfacings will do better.
Is there anything else I should consider?
There is a single paper analysing the British National Joint Registry suggesting that overall mortality is lower in resurfacings versus total hip replacement [21]. This is presently unexplained. Mr McMinn’s team (the developers of the Birmingham Hip Resurfacing) analysed the publicly available data in the UK National Joint Registry comparing Birmingham Hip Resurfacings to all other types of hip replacement for men under 55 with osteoarthritis.
 |
Summary
Although every type of hip replacement represents a compromise, and we do not have the data on which to base a truly informed decision, I recommend:
1. Metal on metal bearings. I specifically recommend the Birmingham Hip Resurfacing system. This is probably the best choice for young men.
2. Ceramicised-metal on plastic. For an older person choosing a THR who does not specifically request or require an alternative, I recommend an Oxinium femoral head on cross-linked polyethylene from the Smith & Nephew company – specifically a R3 acetabular cup and a Synergy non-cemented femoral stem. This is a reliable and proven system.
3. Ceramic on ceramic. For a young person who is not suitable for, or does not want, a resurfacing, I recommend a ceramic on ceramic THR, again the R3 and Synergy combination from Smith & Nephew.
The BHR remains safe despite recalls and problems with other hip resurfacing systems – these problems are due to design features specific to the other systems or to poor positioning of the acetabular components [22] – there is no problem with the principle of hip resurfacing or any problems with the design of the BHR system.
References
1. Henrotin, Y., A. Mobasheri, and M. Marty, Is there any scientific evidence for the use of glucosamine in the management of human osteoarthritis? Arthritis Res Ther, 2012. 14(1): p. 201.
2. Reginster, J.Y., et al., Long-term effects of glucosamine sulphate on osteoarthritis progression: a randomised, placebo-controlled clinical trial. Lancet, 2001. 357(9252): p. 251-6.
3. Malek, I.A., M. Hashmi, and J.P. Holland, Socio-economic impact of Birmingham hip resurfacing on patient employment after ten years. Int Orthop, 2011. 35(10): p. 1467-70.
4. McGrath, M.S., et al., Total hip resurfacing in patients who are sixty years of age or older. J Bone Joint Surg Am, 2008. 90 Suppl 3: p. 27-31.
5. Nizam, I., L. Kohan, and D. Kerr, Hip resurfacing in an 88-year-old patient? Highlighting selection criteria for hip resurfacings in patients older than 65 years. J Arthroplasty, 2009. 24(7): p. 1143 e11-4.
6. McBryde, C.W., et al., The influence of head size and sex on the outcome of Birmingham hip resurfacing. J Bone Joint Surg Am, 2010. 92(1): p. 105-12.
7. Zywiel, M.G., et al., Resurfacing matched to standard total hip arthroplasty by preoperative activity levels - a comparison of postoperative outcomes. Bull NYU Hosp Jt Dis, 2009. 67(2): p. 116-9.
8. Shimmin, A.J. and J.V. Bare, Comparison of functional results of hip resurfacing and total hip replacement: a review of the literature. Orthop Clin North Am, 2011. 42(2): p. 143-51, vii.
9. Lingard, E.A., K. Muthumayandi, and J.P. Holland, Comparison of patientreported outcomes between hip resurfacing and total hip replacement. J Bone Joint Surg Br, 2009. 91(12): p. 1550-4.
10. Mont, M.A., et al., Gait analysis of patients with resurfacing hip arthroplasty compared with hip osteoarthritis and standard total hip arthroplasty. J Arthroplasty, 2007. 22(1): p. 100-8.
11. Costa, M.L., et al., Total hip arthroplasty versus resurfacing arthroplasty in the treatment of patients with arthritis of the hip joint: single centre, parallel group, assessor blinded, randomised controlled trial. BMJ, 2012. 344: p. e2147.
12. Lavigne, M., et al., The John Charnley Award: The functional outcome of hip resurfacing and large-head THA is the same: a randomized, double-blind study. Clin Orthop Relat Res, 2010. 468(2): p. 326-36.
13. Cobb, J., Letter to the editor: The functional outcome of hip resurfacing and large-head THA is the same: a randomized, double-blind study. Clin Orthop Relat Res, 2010. 468(11): p. 3134.
14. Lian, Y.Y., et al., [Changes of the bone mineral density of proximal femur after hip resurfacing arthroplasty]. Zhonghua Wai Ke Za Zhi, 2007. 45(16): p. 1091-4.
15. Smolders, J.M., et al., Changes in bone mineral density in the proximal femur after hip resurfacing and uncemented total hip replacement: A prospective randomised controlled study. J Bone Joint Surg Br, 2010. 92(11): p. 1509-14.
16. Brennan, S.A., et al., Periprosthetic fractures in the resurfaced hip--A case report and review of the literature. Injury, 2013. 44(2): p. 263-5.
17. Weusten, A.J., et al., Internal fixation of a traumatic fracture around a hip resurfacing arthroplasty using the proximal femoral locking compression plate. Acta Orthop Belg, 2012. 78(5): p. 688-93.
18. Whittingham-Jones, P., et al., Internal fixation after subtrochanteric femoral fracture after hip resurfacing arthroplasty. J Arthroplasty, 2010. 25(2): p. 334 e1-4.
19. Baxter, J.A., M. Krkovic, and U. Prakash, Intertrochanteric femoral fracture after hip resurfacing managed with a reverse distal femoral locking plate: a case report. Hip Int, 2010. 20(4): p. 562-4.
20. Tsiridis, E., et al., Periprosthetic femoral fractures around hip arthroplasty: current concepts in their management. Hip Int, 2009. 19(2): p. 75-86.
21. McMinn, D.J., et al., Mortality and implant revision rates of hip arthroplasty in patients with osteoarthritis: registry based cohort study. BMJ, 2012. 344: p.e3319.
22. Grammatopoulos, G., et al., Optimal acetabular orientation for hip resurfacing. J Bone Joint Surg Br, 2010. 92(8): p. 1072-8.
Articles are writter/reviewed/edited by Asia Medical Specialists Copyright ©2017 Asia Medical Specialists Limited. All rights reserved. |
