Hallux Rigidus FAQs
Hallux Rigidus FAQs
Article written by the doctors of Asia Medical Specialists
(Last updatd on: 15th Oct 2020)
What is Hallux Rigidus ?
"Hallux" mean big toe and "Rigidus" mean stiff. It is a medical term describing degeneration of the joint at the base of the big toe – called metatarsophalangeal, or MTP joint. It is the most common site of arthritis in the foot region. It is an important joint, as it has to bend every time you walk and propelling your body forward. Walking can be painful or limited as it is degenerated and stiffened. Most of the time, a bony overgrow (osteophyte) can cause painful bump over the dorsal base of the big toe, resulted in painful impinging shoe-wear.
What is the cause?
Hallux rigidus usually develops in adults at the ages between 30 and 60 years. No exact cause is agreed so far. It can be secondary to previous trauma, or due to the underlying abnormal foot anatomy, abnormal joint surface, surrounding soft tissue imbalance that increase stress on the joint. It is more commonly in distant runner or dancer (Fig. 1) who have repeatedly exert hyperextension of the big toe.
 Fig. 1 Ballet dancer en demi-pointe demonstrating excessive loading on big toe joint. |
How can I be affected?
Patient may experience pain in the joint when you walk, especially as you push-off on the toes when walking up/down stair. There is swelling around the base of big toe especially over the dorsum (top) of the big toe with associated bony bump (Fig. 2).
  Fig. 2 Pseudo-bunion – bunion pain with actually a hallux rigidus case. |
The joint will be stiff at late stage due to the degeneration and the dorsal bony bump (Fig.3).
Fig. 3 Severe/ late hallux rigidus with joint deformity and excessive bone spur. |
How is hallux rigidus diagnosed?
History: pain, stiff, dorsal bunion
Examination: Limited big toe bending especially on upward movement, bump over the top of the base of big toe. Physician will try to differentiate if the symptom is arising from the bony bump, or the joint so as to decide type of surgery if indicated.
X-ray : Narrowing of the MTP joint due to wear of joint cartilage, bony spur (osteophyte) (Fig. 4,5). They are clinically graded into early stage (with the joint still preserved) (Fig. 6) and late stage (with the joint being obliterated) (Fig. 3).
|
What else could it be?
1. Hallux valgus
2. Gout (Fig. 5)
3. Rheumatoid arthritis
4. Infection
5. Post-traumatic osteoarthritis
What are the options of treatment?
Non-surgical treatment:
1. Glucosamine.
2. Traction.
3. Non-steriodal anti-inflammatory drug (NSAID) such as ibuprofen may help reduce the active swelling and pain relief.
4. Ice packs or taking contrast baths may help for short period of time.
5. Shoe modification with widen toe box to accommodate the bump, stiff-soled shoe with a rocker bottom design may help to prevent bending force on the joint. Orthotic with a steel shank or metal brace in the sole can be measured with similar action. These are not effective to stop the condition from progressing but just symptomatic relief.
6. Injections –
• Steroid
• hyaluronic acid
Surgical treatment
Different types of surgical treatment are commonly practiced depending on the clinical examination and radiological grading of degeneration.
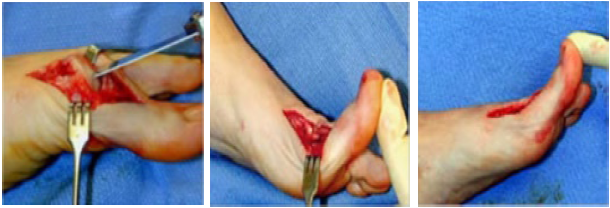
1. Cheilectomy operation [1]. This is a simple operation to remove the osteophytes that limit the range of motion (Fig. 7,8). It improves range of motion for wearing higher heel shoes or for running, and, though it often reduces pain, this is not guaranteed. It takes 3 months to recover 80% and 6 months to fully recover. Naturally, this does not alter the natural history of the underlying problem of arthritis; it merely reduces the pain from impingement of the osteophytes, which are caused by the arthritis. The potential problem is risk of further joint degeneration and requires further surgical procedure, it is however a buy-time procedure.
|
2. Autologous interposition arthroplasty using a free ipsilateral gracilis tendon graft is for patients with severe hallux rigidus with moderate to high activity levels and who do not wish to undergo fusion [2].
3. Fusion operation [1]. This is a procedure to remove the joint and join the bones of the foot and toe together. This reliably removes pain and allows one to return to running.This is a procedure indicated for those with pain due to both bony spur and the joint (Fig. 3). It is more assuring procedure as the diseased joint is converted to a stable one-piece bone. The trade-off is the big toe become stiff, but we usually fused it in a physiological position for walking. A plate and screws (Fig. 9) are used to stabilise the fixation for the bone surface to heal by 6-8 weeks.
|
4. Arthroplasty (excision of the whole joint +/– replacing with a spacer or an artificial prosthesis) is a joint replacement, which significantly reduces pain and allows good function. It may have a limited life of approximately 10 years and require revision or a fusion operation later. This is an alternative procedure to arthrodesis for those older people who place few functional demands on the feet. It is not well accepted as the potential risk of prosthesis complications e.g. wear, dislocation, loosening, etc.
What are the risks of surgery?
Surgery is usually done under general / spinal / regional anaesthesia. This includes general risk of anaesthetic drug and specific risks which our anaesthetist will explain to you before the operation accordingly.
General surgical risks include infection, nerve injury, tourniquet risk, swelling and stiffness. Specific risk for Cheilectomy : recurrence / progression of symptom.
Specific risk for Arthrodesis : stiff joint, implant loosening, impingement, non-union, delayed union. Shortening of big toe.
Specific risk for Arthroplasty : prosthesis dislocation / loosening.
Are there other alternatives?
Steriod injection is done by some GP / Surgeon, but it is only a temporary effect and potential risk of infection, bony necrosis.
Minimal invasive with percutaneous screw fixation is advocated but only short-term and small series report.
What is the post-operative planning?
Cheilectomy : since there is no joint procedure done but only bone spur excision, immediate return to normal walking is allowed. The wound will usually take 10-14 days to heal. Early passive big toe movement is advised to prevent the joint stiffness is the main physiotherapy recommended. Takes months to settle.
Arthrodesis : This requires longer rehabilitation as it involves timing for stable bone growth which usually takes 6-8 weeks. Patient will be protected with cast immediate post-operation and educated for non-weight bearing walking during initial 6 weeks. Radiological check will make at around 6 weeks to confirm if full weight bearing walking is advisable. Patient will be unable to wear high-heeled shoes due to the stiffened big toe (or we sometimes modify the position of fusion so as to tailor the patient's reasonable need in terms of shoewear)
Arthroplasty : the rehabilitation is similar as arthrodesis but early mobilisation is essential to keep with the surgical benefit. Weight bearing is avoided for soft tissue stabilisation which usually takes 4-6 weeks.
When can I return to work?
It depends on the type of procedure as well as the occupation requirement of the individual. 2-6 weeks as mentioned under different procedures.
Can I return to sport?
Yes with both cheilectomy and arthrodesis but with limited big toe flexibility in the later case.
To understand more about the disease, please contact us at info@asiamedical.hk or call us at +852 2521 6830.
References
1. Coughlin MJ, Shurnas PS. Hallux Rigidus. Surgical Techniques (Cheilectomy and Arthrodesis). J Bone Joint Surg Am. September 1, 2004 2004;86(1_suppl_2):119-130.
2. Miller D, Maffulli N. Free gracilis interposition arthroplasty for severe hallux rigidus. Bull Hosp Jt Dis. 2005;62(3-4):121-124.
3. Marx RC, Mizel MS. What’s New in Foot and Ankle Surgery. J Bone Joint Surg Am. April 1, 2008 2008;90(4):928-942.
4. Current Procedural Terminology. Chicago, IL: American Medical Association; 2007.
| Copyright ©2017 Asia Medical Specialists Limited. All rights reserved. |