防治中風的新概念與最新發展
防治中風的新概念與最新發展
written by doctors of Asia Medical Specialists
(Last update on: Oct 28th 2020)
傳統對「腦血管病變」的概念近年已被「腦中風」取替。與突發性心臟病一樣,腦中風是屬於突發性的心血管疾病,亦有相類似治療概念。血管神經外科醫生亦會先選擇腦內血管介入療法,而不是經靜脈注射溶血劑。腦內血管介入療法須於症狀出現後的八小時內進行。這就是治療腦中風最新的黃金八小時概念。
完整英文版本已經上載,中文版本即將更新。
摘要
“腦血管意外”的舊概念最近被“腦部攻擊”的新概念所取代。就像心臟病發作一樣,腦發作也是一種急性心血管疾病。心臟病發作和腦部發作的病因相似。心臟病發作的治療概念也適用於腦部發作。對於
心臟病發作,心髒病專家更喜歡使用經皮冠狀動脈介入治療,即心臟PCI,而不是靜脈注射重組組織纖溶酶原激活劑(例如iv rtPA)。症狀發作後的12小時內必須進行心臟PCI。因此,IV rtPA是心髒病發作的第二線治療,僅在PCI不可用時才提供。
類似的概念也適用於腦部發作。血管神經外科醫生也更喜歡經皮腦介入術(Neuro-PCI),而不是靜脈rtPA。症狀發作後的8小時內必須執行Neuro-PCI。因此,這是用於腦部攻擊的全新Golden-8小時概念。如今,Neuro-PCI是美國大多數綜合卒中中心提供的一線標準治療。 Golden-3-小時內的Iv rtPA被認為是第二線治療,僅當Neuro-PCI不可用時才提供。
|
中風的新概念
腦血管意外的舊觀念和對逐漸的神經系統惡化以及最終的殘疾甚至死亡狀態的命運的接受應該發生革命性的變化。新的術語“大腦發作”意味著中風不是偶然的。就像心髒病發作一樣,中風是可以預防,治療甚至治癒的,不會給患者帶來任何神經系統缺陷。中風的治療方法與心髒病發作類似。將來,患有急性缺血性中風的患者將更不會痛苦[1,2]。
什麼是中風?
術語“中風”是指由於血管原因引起的神經功能障礙的突然發作。中風有兩種類型:缺血性中風佔西方世界所有中風的約87%(香港約佔70%)。出血性中風解釋了其餘的13%(香港為30%)。但是出血性中風的死亡率高於缺血性實體。它佔所有中風死亡的30%以上。Pathophysiology
不論年齡,種族或性別,中風都會有機會發生在任何人身上。在缺血性中風期間,大腦中的血管被阻塞。阻塞會擾亂血液流動,阻止氧氣輸送到受影響的大腦區域。缺氧的腦組織部分變得“震驚”,不再正常工作,從而導致中風症狀。
時間就是大腦
急性缺血性中風(AIS)是嚴重的醫療急症。快速介入至關重要。每分鐘大血管中風得不到治療,就會損失多達190萬個神經元(每秒損失32,000個神經元,每小時損失1.2億個神經元),失去140億個突觸,失去7.5英里的有髓纖維。中風得不到治療的時間越長,永久性神經損傷的可能性就越大。如果延遲治療,則“腦梗死”會導致關鍵腦細胞的額外死亡,從而降低治療的潛在益處。短時間治療對於增加良好恢復的機率絕對至關重要。大約三個小時後,腦細胞將遭受不可逆轉的傷害,通常導致其死亡。這就是為什麼僅在中風發作後三小時才進行rtPA溶栓治療的原因。因此,時間確實是大腦[3].
中風對流行病學和社會經濟影響
- 香港每年大約有18,000例中風病例。每年大約有795,000名美國人經歷新的(610,000)或經常性(185,000)中風。
- 中風是美國第三大死亡原因,僅次於心髒病和癌症。據估計,每年約有60,000美國人死於中風。它導致全世界10%的死亡[4]。
- 由於人口老齡化,預計未來幾十年中風的發病率將上升。它可能很快成為全世界最常見的死亡原因。[5].腦卒中的發病率從30歲開始呈指數增長,病因因年齡而異[6]。
- 中風是導致長期嚴重殘疾的主要原因
- 中風是住院長期成人醫療保險報銷的第一原因。現在,在美國,每年的中風總費用超過630億美元。 2010年中風的直接和間接費用估計為737億美元。
- 目前有超過300萬人患有中風,其個人和經濟損失是巨大的。
- 除身體和經濟負擔外,中風還給患者及其家人造成巨大的心理影響
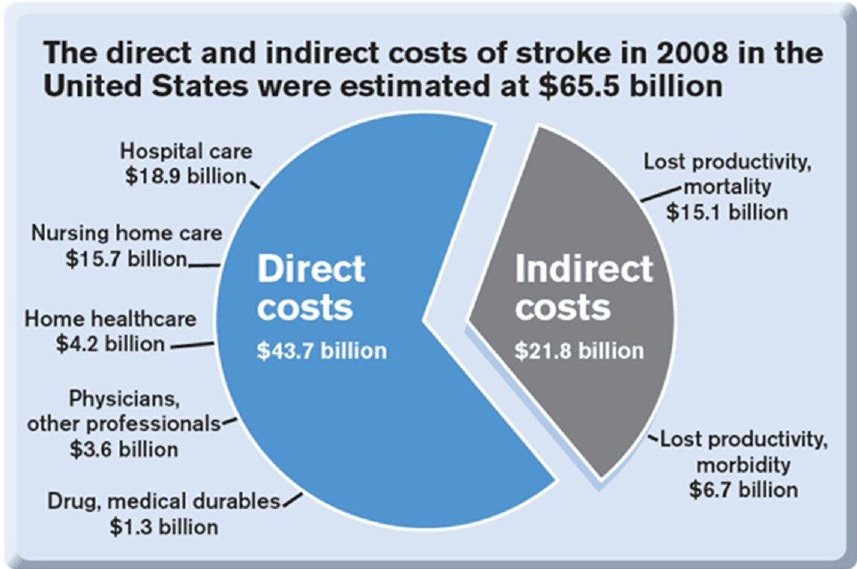 Fig. 2 Total stroke cost in US |
The New Concept of Stroke Management
The new concept emphasises screening of stroke risk, the control of risk factors and the prevention on brain attack; public education on stroke symptoms allowing rapid recognition and seeking of emergency help; and, most importantly, fast-track treatment of acute brain attack during the golden hours of the therapeutic window.
QT3
Question, Screening, Prevention, Time, Place, Person, 3D8P
(QSP-TPP-3D8P)
Screening for Stroke: Question, Screening, Prevention
- Question: Ask patients questions: their own estimation of life time stroke risk (reflecting their awareness of own health and family history)
- CLIS Screening: (Clinical screen, Laboratory screen, Image screen).
a. Clinical screen:
i. SDHHH History (personal and family): Stroke, Diabetes, Hyperlipidemia, Hypertension, Heart disease.
ii. BHCBP Examination: Body Mass Index, Heart status, Carotid artery for bruit, Blood pressure, Pulse for atrial fibrillation.
b. GOCO Laboratory screen: Glucose level, (Oil) Lipid profile, Clotting profile , (Organs) Liver and Renal function.
c. Image screen: Magnetic Resonance Imaging of brain, brain vessels and carotid and vertebral arteries. - Prevention of stroke or Risk factors control: (Up to 80% of strokes are preventable; you can prevent a stroke.
a. DEWCAD Lifestyle Modification: Diet (Calorie intake, Glucose, Fat, Salt consumption) [7], Exercise, Weight, Cigarettes 8 , Alcohol 9, Drug (Oral contraceptive pills, soft drugs [10])
b. POGAS Medical Therapy: Drug for Blood pressure control11, Cholesterolaemia [11], Glucose control for diabetes [12], Atrial Fibrillation (Anticoagulant)13, Stroke in the past (Antiplatelet)
c. Structural abnormalities with or without symptoms: Refer to vascular nerosurgeon for Prophylactic Neurosurgery Percutaneous Cerebral Intervention (Neuro-PCI)
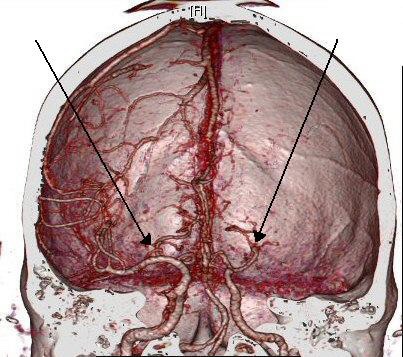
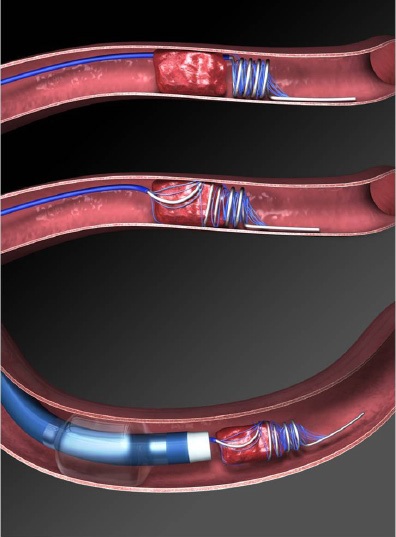
i. Cervical arteries stenosis: i.e. carotid stent for carotid stenosis [14].
ii. Intracranial vascular anomaly: e.g. hypoplastic vessels in circle of Willis: only acknowledge and aware.
iii. Intracranial vascular stenosis: i.e. Intracranial vascular stent for Middle Cerebral Artery (MCA) stenosis [15].
iv. Cerebral aneurysm or arteriovenous malformation: Endovascular embolisation therapy for reducing the risk of haemorrhagic stroke.
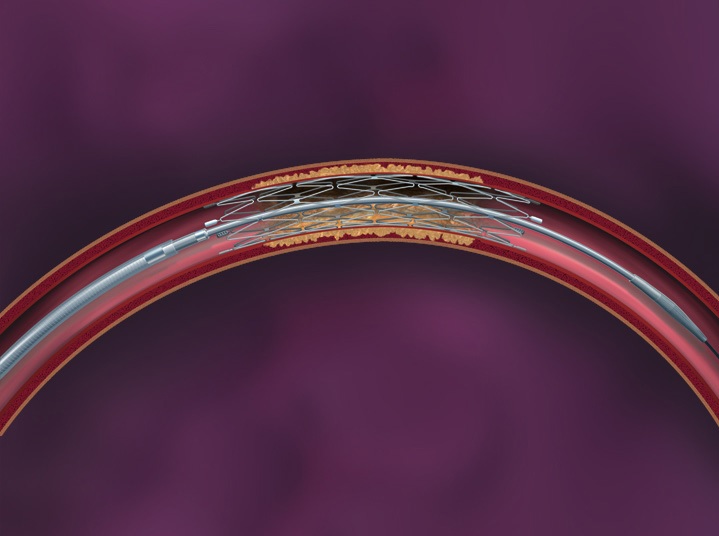 Fig. 3 The Wingspan system of intracranial vascular stent |
Management of Acute Stroke (TPP-3D8P)
Time--Place--Person--3 Golden hours Drug or PCI—8 Golden Hours only PCI (TPP-3D8P)
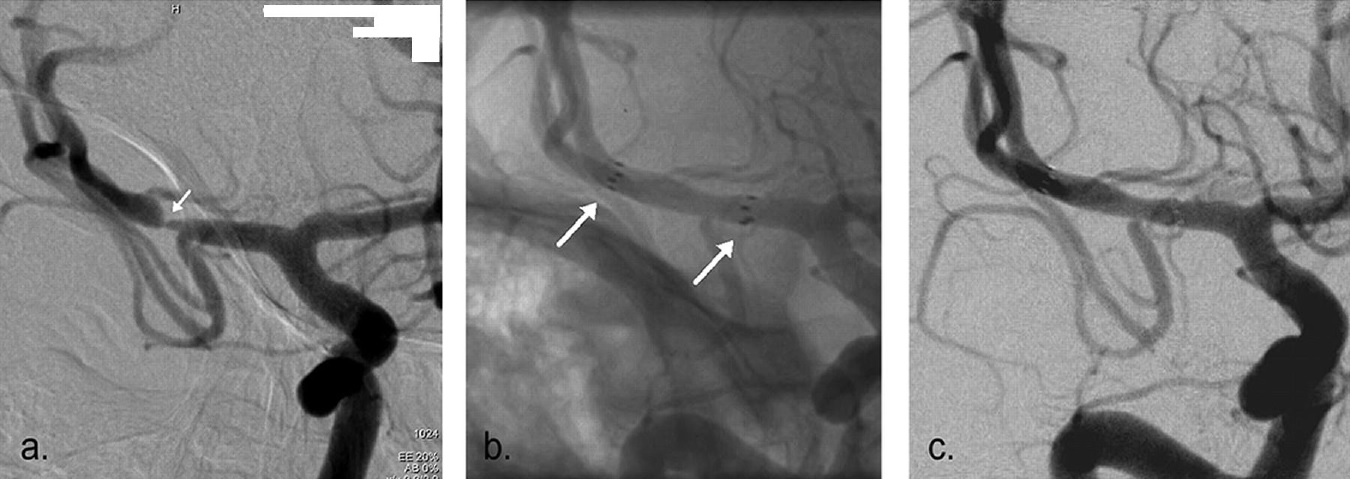 Fig. 4a The Pre-stenting angiogram (DSA) showing right MCA stenosis, b. stent-in-situ with stent marker (white arrow), c. the post-stenting DSA |
1. Time:
- Establish the exact time of symptoms onset or the time when patient was last seen to be normal. Recognition of stroke symptoms i.e. facial appearance, limbs weakness, speech problem,visual and sensory disturbance, gait and coordination, orientation and consciousness, etc.
- Promptly seek for emergency help during the Golden-3-Hours therapeutic window.
2. Place:
Seek immediate medical assessment and treatment in Hospital equipped with CT scanner, MRI scanner and Angiogram machine [16].
3. Person:
Seek help from vascular neurosurgeon who can provide comprehensive treatment and who can manage the complications associated with ischaemic stroke and its treatment.
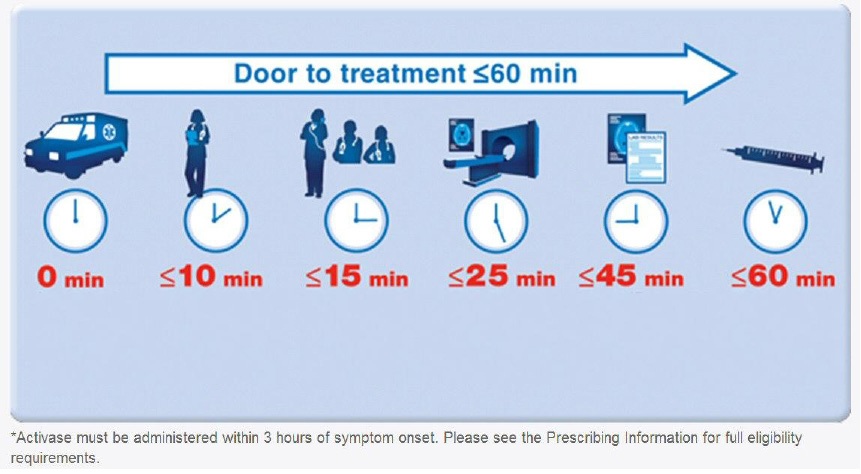
4. 3-Golden-hours Drug or PCI:
- After clinical assessment of the contraindications for intravenous recombinant tissue plasminogen activator (iv rtPA or ‘Activase’), the fibrinolytic drug may be given as the first line treatment if the option of Neuro-PCI is not available.
- Most (>90%) of the acute ischaemic stroke patients will not benefit from iv rtPA due to: i. late presentation to emergency room (more than 2 hours after symptom onset), ii. fall into the exclusion criteria of iv rtPA, iii. delayed diagnosis in emergency rooms or clinical wards due to misinterpretation of CT scan.
- The benefit of iv rTPA should weighted against its associated high risks. Properly informed consent is vital [17, 18].
|
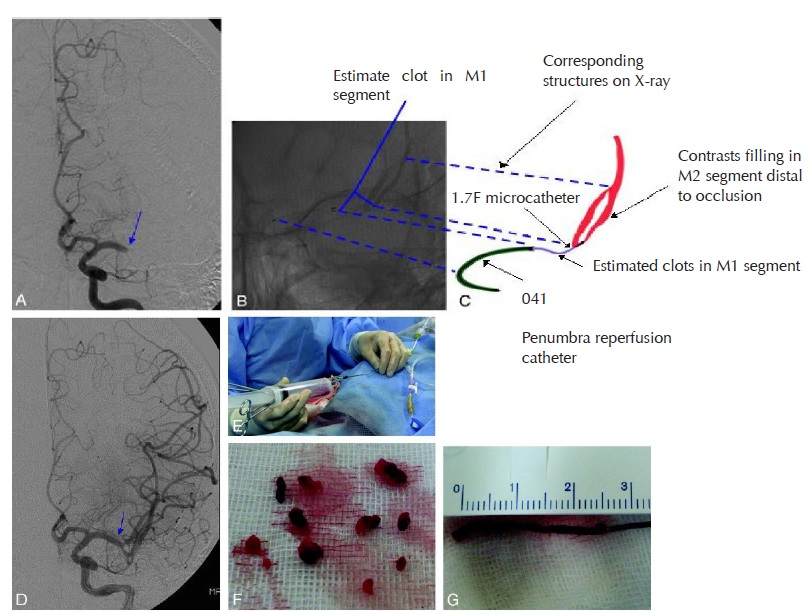
5. 8-Golden-Hours only PCI (Neurosurgical Percutaneous Cerebral Intervention)
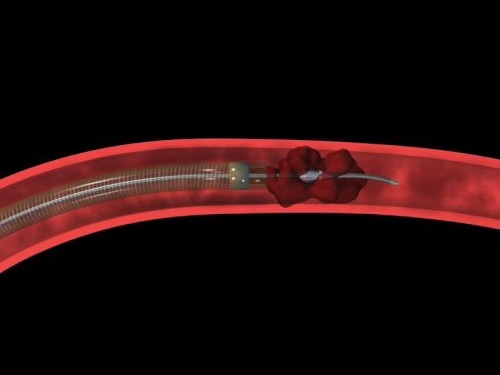
- Neuro-PCI achieves brain revascularisation by mechanical thrombectomy under fluoroscopic guidance of cerebral angiograms. A micro-catheter is passed up to the occluding thrombus in intracranial vessels. The thrombus or embolus is removed by the device using mechanical breakage and aspiration.
- Intra-arterial fibrinolysis i.e. ia rtPA injected at the site of thrombosis, improves outcomes in acute ischemic stroke [19] .
- Intra-vascular stent may be deployed if concomitant vascular stenosis exists.
- Within the Golden-3-hours, Neuro PCI can revascularise the brain cells and minimise the central infarction core. Patients may have full recovery without any neurological deficit.
- Within the Golden-8-Hours: From the therapeutic window of the 4th hour to the 7th hour, Neuro-PCI revascularisation can salvage brain cells in the peripheral ischaemic region called the Penumbra Zone and minimise the volume of brain infarction. Thus the overall morbidity and mortality of ischaemic stroke is reduced.
- Neuro-PCI is also indicated for patients who were unable to receive iv rtPA due to contraindications or for whom the drugs were ineffective [20, 21, 22, 23].
|
Salvage Neurosurgery
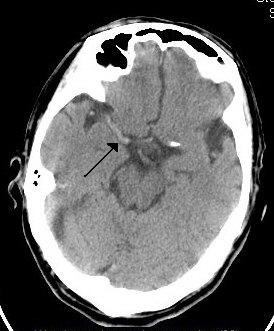
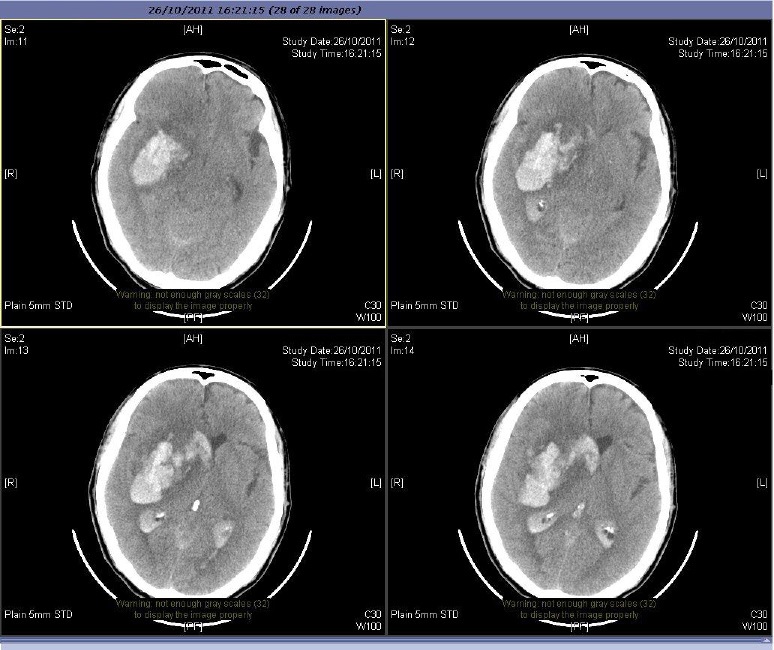
1. Surgery for bleeding complication of iv rtPA
Around 6% of iv rtPA treated patients develop symptomatic intracranial bleeding that cause more disastrous brain damage [24]. Salvage neurosurgery is difficult due to rtPA caused bleeding tendency. Though surgery may be lifesaving, patients may be severely disabled or even vegetative.
|
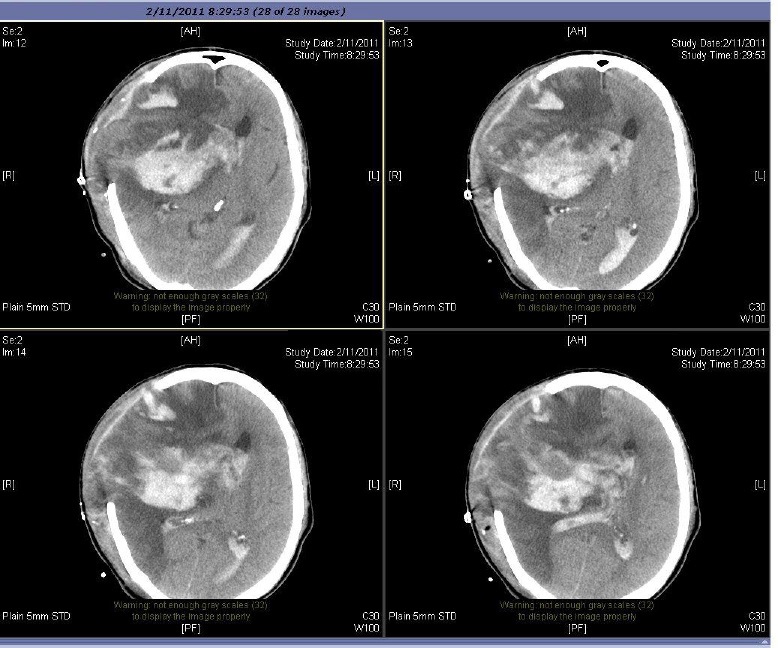
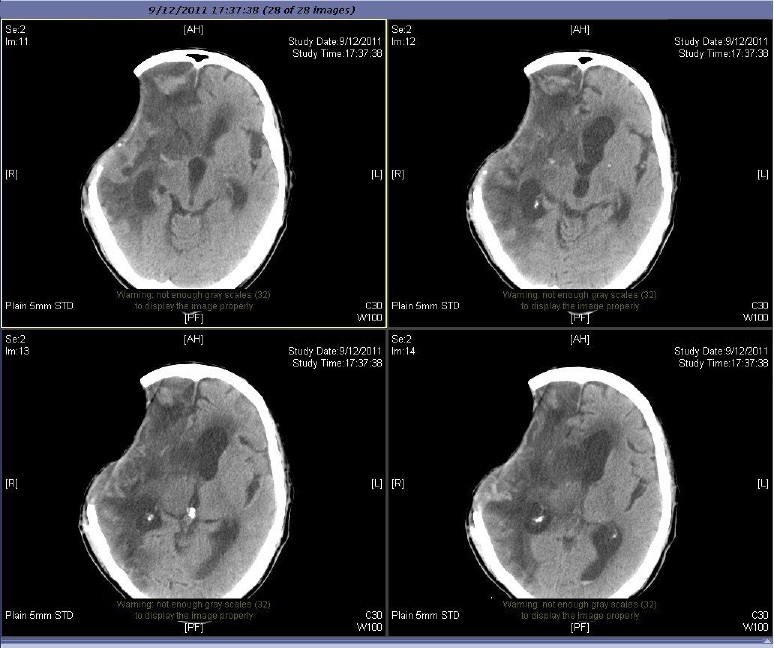
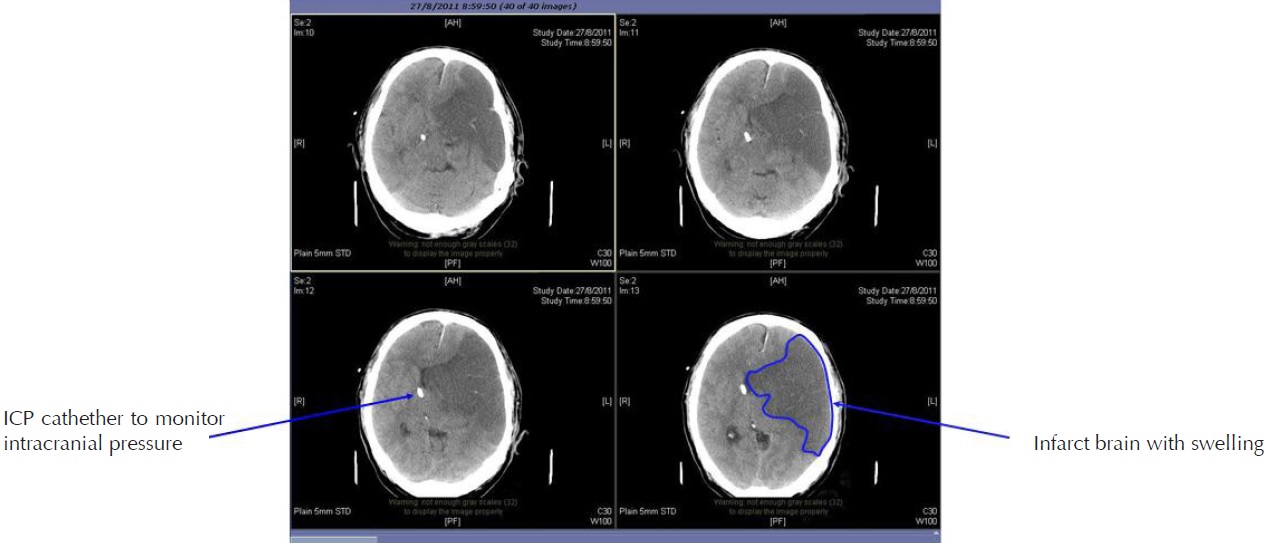
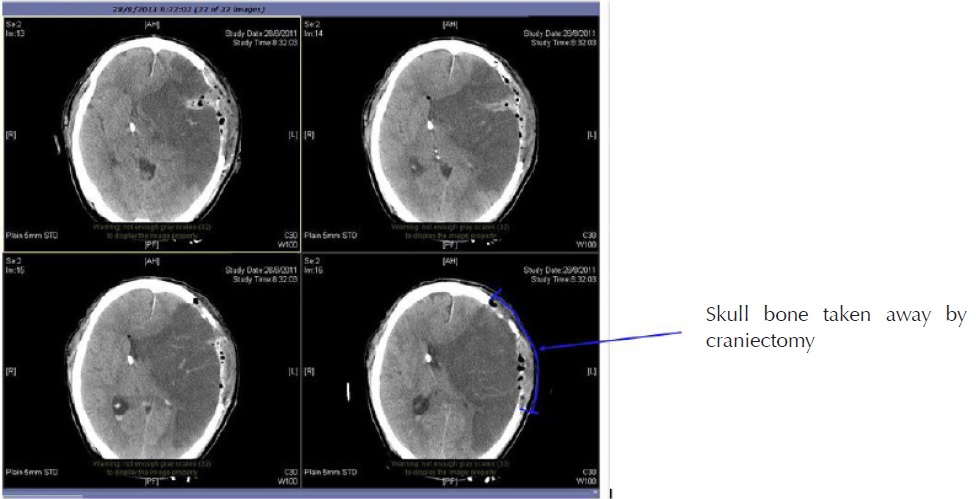
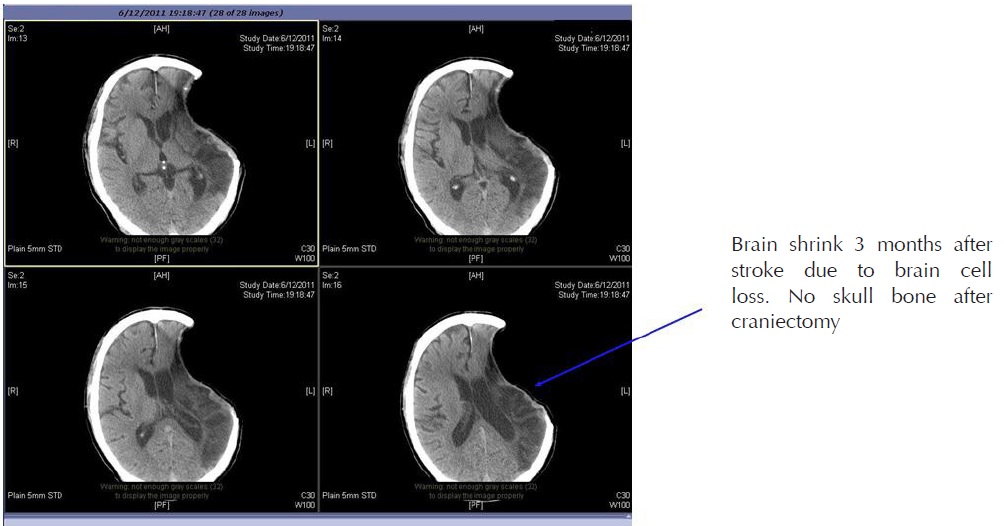
2. Cranial Decompressive Surgery: Craniectomy +/- Lobectomy
Large territory strokes can cause significant oedema of the brain with secondary brain injury in surrounding tissue. This phenomenon is mainly encountered in strokes of the middle cerebral artery territory, and is also called “malignant cerebral infaction” because it carries a dismal prognosis. Relief of the pressure may be attempted with medication, but some require decompressive craniectomy (temporary surgical removal of the skull) +/- lobectomy with excision of infarcted brain tissue. This confers a marked improvement in the risk of death, although most survivors are disabled [25].
|
References
1. World Health Organisation (1978). Cerebrovascular Disorders (Offset Publications). Geneva
2. Kidwell CS, Warach S (December 2003). “Acute ischemic cerebrovascular syndrome: diagnostic criteria”. Stroke 34 (12): 2995–8
3. Saver JL (2006). “Time is brain - quantified”. Stroke 37 (1): 263–6
4. The World health report 2004. Annex Table 2: Deaths by cause, sex and mortality stratum in WHO regions, estimates for 2002. Geneva
5. Murray CJ, Lopez AD (1997). “Mortality by cause for eight regions of the world: Global Burden of Disease Study”. Lancet 349 (9061): 1269–76.
6. Ellekjær, H; Holmen J, Indredavik B, Terent A (November 1, 1997). “Epidemiology of Stroke in Innherred, Norway, 1994 to 1996 : Incidence and 30-Day Case-Fatality Rate”. Stroke 28 (11): 2180–2184
| ©2017 Asia Medical Specialists Limited. All rights reserved. |